Translate this page into:
Congenital Ovarian Cyst: A Report of Two Cases
Address for correspondence: Dr. Manjula Jain, E-mail: drmeenupujani@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A congenital ovarian cyst is a rare clinical entity which can be diagnosed during antenatal ultrasonography. Although rare, it is the most common cause of intra abdominal cyst in female fetal abdomen. These are benign, functional cysts which result from enlargement of otherwise normal follicles during third trimester or early neonatal period. Since most of them follow a benign course, they have an excellent prognosis especially if the cyst is isolated, unilateral, and unilocular. Here we report two cases of unilateral, simple, uncomplicated ovarian cysts in neonates managed by cystectomy (open).
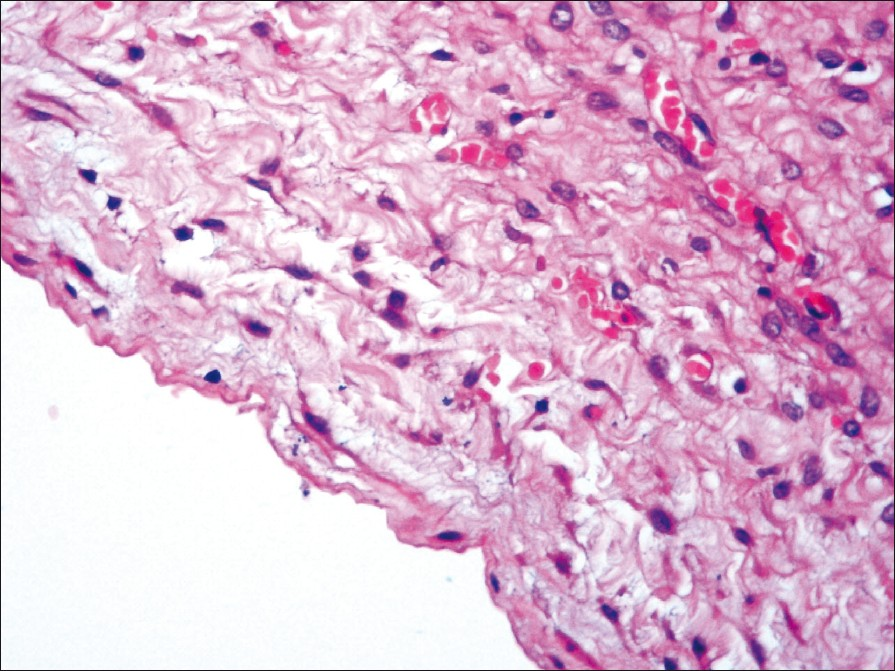
Case 1: A 28-year-old female delivered a female baby by normal vaginal delivery at term. Antenatal ultrasound during the third trimester revealed a large thin-walled unilocular abdominal cyst measuring 6.2×6.1 cm in the right side of fetal pelvis. On the 10th day of postnatal life, the baby presented with mass felt per abdomen. A computerized tomography scan (CT scan) demonstrated a well-defined hypodense lesion measuring 6.8×6.7×4 cm in the pelvis suggesting an ovarian cyst. Cystectomy was performed. Grossly, a large smooth walled gray white unilocular cyst, 6 cm in diameter filled with straw colored serous fluid, was seen. Microscopy revealed a corpus luteal cyst [Figure 1].

- Ovarian cyst wall composed of ovarian stroma, lined by luteal cells (H and E, ×400)
Case 2: A 25-year-old female delivered a female baby by a caesarean section. No antenatal records were available. On the third postnatal day, the baby presented with distension abdomen. CT scan showed a huge (11.7×11.5×5cm) unilocular cyst arising from left side of pelvis, occupying whole of abdomen. Due to its large size, immediate resection was performed. Grossly, strips of the thin smooth cyst wall were received. Multiple sections examined microscopically revealed a cyst wall composed of ovarian stroma enclosing dilated and congested blood vessels. However, no lining epithelium could be identified in the multiple sections studied [Figure 2]. A possibility of a follicular/simple serous cyst was suggested.
- Ovarian cyst wall composed of ovarian stroma and congested blood vessels, no lining epithelium seen. (H and E, ×400)
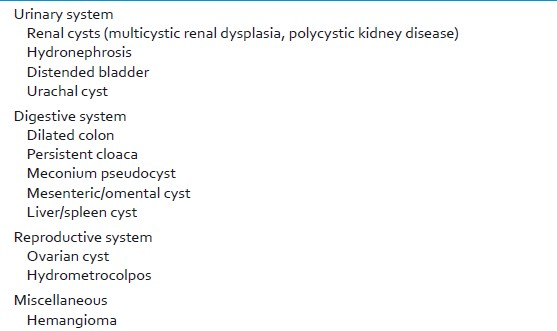
A variety of cystic masses can be seen in fetal/neonatal abdomen [Table 1]. Out of the listed causes, ovarian cysts are the most common intra-abdominal cyst in female neonate. It is a relatively rare condition with approximately 100 neonatal cases reported in the literature. The first case of an ovarian cyst was reported in 1889 in a stillborn premature.[1] In 1942, Bulfamonte reported the first case of a successfully treated ovarian cyst during the neonatal period.[2] The first antenatal observation of ovarian cyst was done by Valenti.[3]
The genesis of fetal/ovarian cysts is controversial. It results from fetal exposure to maternal gonadotrophins and is observed in newborns whose mothers have increasing levels of HCG (diabetes mellitus, Rh isoimmunisation, toxaemia).[4] A precocious FSH peak between 20--30 weeks of gestation and abnormal HCG peak due to disorders of theca interna may also be contributory. Prematurity and fetal hypothyroidism are also associated.[3]
The majority of the ovarian cysts are benign cysts of germinal/graafian origin such as follicular, theca-lutein cyst, corpus luteum cyst, and simple cyst in which lining epithelium is destroyed. These are benign, functional cysts which result from enlargement of otherwise normal follicles present in third trimester and early neonatal period. Most of the cysts are unilateral and unilocular. The size may vary from small to giant cystic masses occupying the entire abdomen. Most of the ovarian cysts are asymptomatic, or the symptoms are nonspecific. A large cyst may cause urinary tract obstruction, thorax compression with pulmonary hypoplasia, and even sudden death.[5] These cyst have been classified by Nussbaum into simple/uncomplicated and complex/complicated (fluid debris level, clot, septae echogenic wall).[6] Common complications include torsion (50--78%), rupture, hemorrhage, compression of other viscera, autoamputation.[34] With increased use of prenatal ultrasonography, the detection rate for these cysts has increased considerably. Up to 34% of the fetuses may have antenatally detectable cysts.[5] Few case reports documenting neonatal ovarian cysts have been reported.[17–9] Few of the cases documented in the literature were complicated cysts presenting with torsion[1] unlike both of our cases which were unilateral, simple without any associated complications.
Spontaneous regression occurs in 25-50% of cases and is more frequent with smaller cysts.[10] It has been proposed that postdelivery, as the anterior pituitary starts the negative biofeedback mechanism, the abnormal gonadotrophin secretion is discontinued, and many of these cysts regress spontaneously although regression may take up to 10 months.[4] Regarding management, small simple cysts under 4 cm in diameter can be kept under observation by serial ultrasonography scan. However, all complicated ovarian cyst and simple cysts >5 cm diameter should be treated surgically. Minimal access surgery/laparoscopy, being well tolerated by neonates, can be used for aspiration, marsupilization, cystectomy, and oophorectomy[11] or the more conventional open approach can be used.
REFERENCES
- Antenatally diagnosed neonatal ovarian cyst with torsion. Indian J Pathol Microbiol. 2011;54:228-9.
- [Google Scholar]
- Ovarian cysts in the newborn. Am J Roentgenol Radium Ther Nucl Med. 1972;116:664-72.
- [Google Scholar]
- Ovarian ultrasonography in newborns and infants. Paediatr Endocrinol. 2008;3:65-70.
- [Google Scholar]
- Neonatal ovarian cysts.sonographic-pathologic correlation. Radiology. 1988;68:817-21.
- [Google Scholar]
- Laparoscopic management of neonatal ovarian cysts. J Indian Assoc Pediatr. 2005;10:100-2.
- [Google Scholar]
- Antenatally diagnosed ovarian cyst with torsion managed laparoscopically. J Indian Assoc Pediatr Surg. 2008;13:28-9.
- [Google Scholar]
- Ovarian enlargements in the first year of life: Review of 45 cases. Ann Surg. 1965;161:372-7.
- [Google Scholar]
- Intra abdominal cystic swelling in children- laparoscopic approach, our experience. J Indian Assoc Pediatr Surg. 2003;8:213-7.
- [Google Scholar]
- Minimally invasive surgery in neonates and infants. J Indian Assoc Pediatr Surg. 2010;15:2-8.
- [Google Scholar]




