Translate this page into:
Pyogenic liver abscess due to Burkholderia pseudomallei in immunocompetent patient from Garhwal region of Uttarakhand – A case report
*Corresponding author: Vinita Rawat, Department of Microbiology, Veer Chandra Singh Garhwali Government Institute of Medical Science and Research, Srinagar, Uttarakhand, India. drvinitarawat31@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Suryakant, Goswami P, Devrari J, Yadav L, Rawat V. Pyogenic liver abscess due to Burkholderia pseudomallei in immunocompetent patient from Garhwal region of Uttarakhand – A case report. J Lab Physicians. 2024;16:567-9. doi: 10.25259/JLP_131_2024
Abstract
We report a case of liver abscess due to Burkholderia pseudomallei in a 45-year-old, non-diabetic patient from the Garhwal region of Uttarakhand. The patient reported chief complaints of abdominal pain and fever. Ultrasonography and contrast-enhanced computed tomography of the whole abdomen were suggestive of the left liver lobe abscess. Pus was aspirated from the abscess and sent for culture and sensitivity. Growth on the culture plate was identified as B. pseudomallei; the patient was then treated with appropriate antibiotics and discharged in stable condition. Diagnosis of pseudomallei infection requires a high index of suspicion among clinicians as well as laboratory specialists. Early identification of organisms helped clinicians initiate appropriate management in our case.
Keywords
Melioidosis
Liver abscess
Burkholderia pseudomallei
INTRODUCTION
Liver abscesses are endemic in developing countries, especially in tropical countries such as India. Pyogenic liver abscess is life-threatening and remains a formidable diagnostic and therapeutic problem and constitutes 80% of liver abscesses.[1] Melioidosis is a systemic infection caused by Burkholderia pseudomallei. In India, most of the reports on Melioidosis are from the southern coastal region, and this entity is very rare from the hilly region of the north (Uttarakhand).[2] We report a case of liver abscess due to B. pseudomallei in a 45-year-old, non-diabetic patient from the Garhwal region of Uttarakhand.
CASE REPORT
A 45-year-old male presented to the surgery outpatient department in 1st week of April 2024 with a chief complaint of abdominal pain for 2 weeks. The pain was progressive in nature and associated with fever (on and off). On physical examination, he was icteric, and tenderness was present in the epigastric and right hypochondrium region. He was advised ultrasonography (USG) and contrast-enhanced computed tomography (CECT) whole abdomen. USG and CECT reports revealed a heteroechoic area measuring 4.8 × 4 × 3.6 cm and a hypodense lesion in the left lobe of the liver, and moderate hepatomegaly with mild free fluid in the pelvic cavity, respectively, suggestive of liver abscess [Figure 1]. He was then admitted to the surgery ward and advised routine investigations. A farmer by occupation, he had a history of walking barefoot.
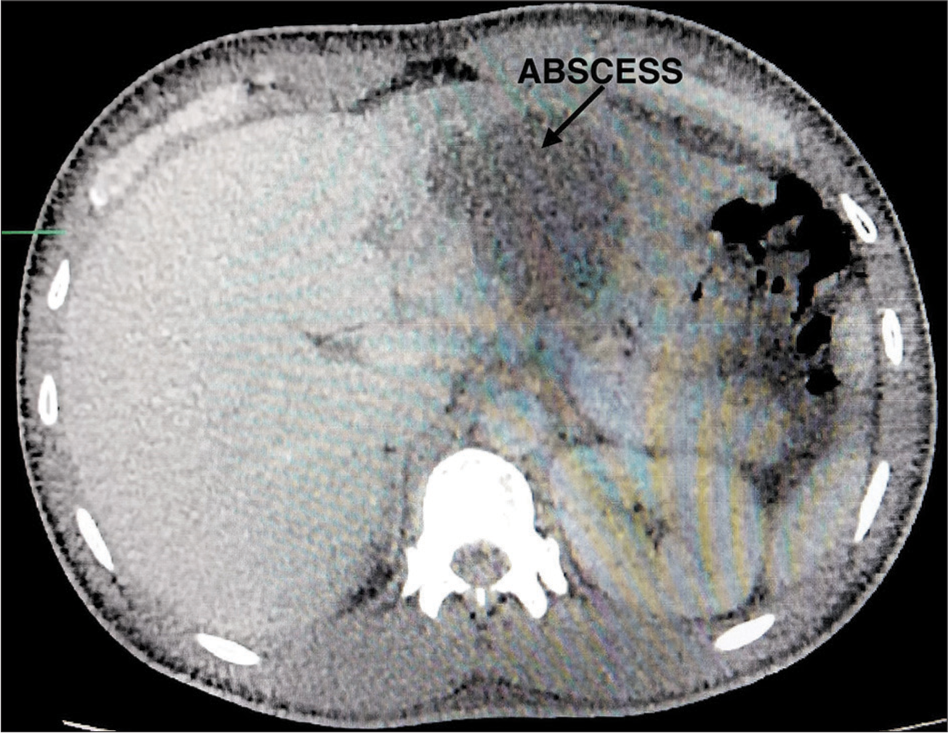
- Contrast-enhanced computed tomography of abdomen demonstrating heteroechoic area measuring 4.8 × 4 × 3.6 cm and hypodense lesion in the left lobe of liver, moderate hepatomegaly with mild free fluid in the pelvic cavity.
Laboratory reports showed white blood cell = 15 × 103/μL, neutrophil 81%, red blood cell = 4.47 × 106/μL, hemoglobin (Hb) = 13.6 g/dL, random blood glucose = 110 mg/dL, blood urea = 14 mg/dL, serum creatinine =0.8 mg/dL, serum bilirubin (total) = 0.9 mg/dL, serum bilirubin (direct) = 0.9 mg/dL, serum albumin = 3.0 gm/dL, serum glutamic-oxaloacetic transaminase = 37 U/L, alkaline phosphatase = 117 U/L, HBs antigen, and total anti-hepatitis C were non-reactive, and human immunodeficiency virus infection was also ruled out.
A provisional diagnosis of the left liver lobe abscess was made, following which pigtail catheter insertion was done under local anesthesia, and pus was aspirated from the abscess and sent to the microbiology department for culture and sensitivity. Empirical therapy with injection of piperacillin-tazobactam was started. Pus was inoculated on 5% sheep blood and MacConkey agar; after 48 h of incubation culture, small, smooth, creamy white colonies were seen on blood agar [Figure 2], and after 72 h, wrinkled colonies were observed. Gram staining revealed Gram-negative bacilli with a typical safety pin appearance. The oxidase test was positive, arginine was hydrolyzed, and the isolate was resistant to polymyxin, which was suggestive of B. pseudomallei (later on identified by VITEK2). Isolate was sensitive to levofloxacin, ceftazidime, meropenem, minocycline, and cotrimoxazole.
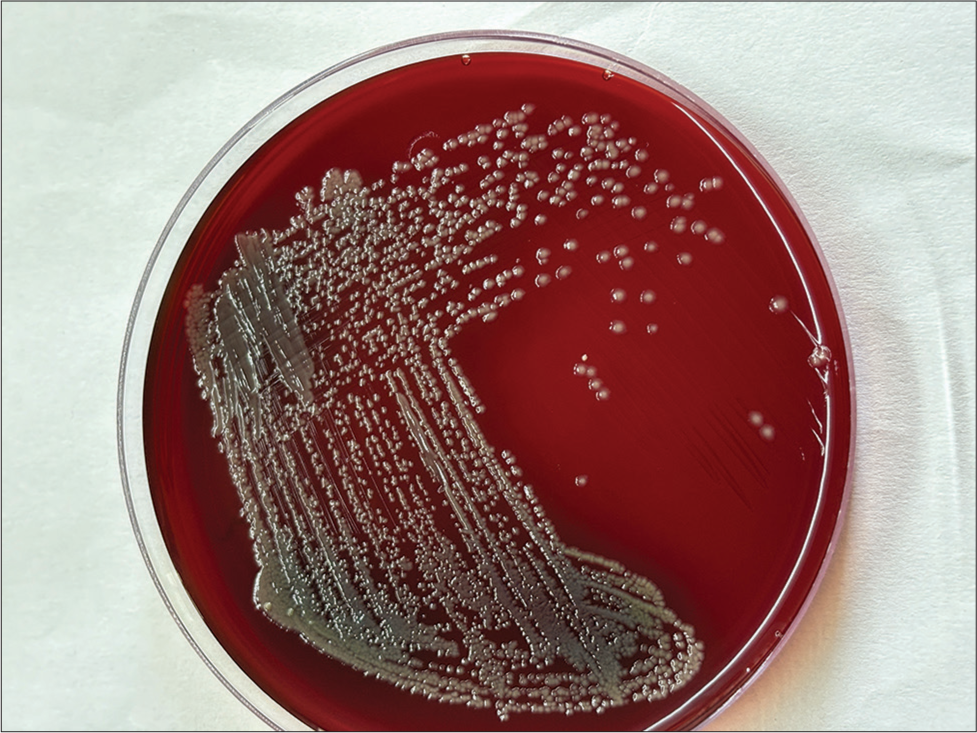
- Colony of Burkholderia pseudomallei bacteria on sheep blood agar after 48 h of incubation.
Antibiotic therapy was changed to intravenous meropenem and continued for 2 weeks. The pigtail catheter was removed after 2 weeks and tab. cotrimoxazole for 20 weeks was prescribed, and the patient was discharged under satisfactory conditions. The patient was advised to follow up. After this, he followed up in the months of June and July 2024 and showed better improvement. Then, from August 2024, there was a loss of follow-up.
DISCUSSION
Melioidosis is a systemic infection caused by the environmental bacteria B. pseudomallei. It is also known as the “Great Imitator,” causing diagnostic dilemmas and clinical spectrum ranging from subclinical infection, localized superficial or deep abscess, and severe pneumonia to fulminant sepsis.[3]
In India, in the past decade, there has been an increasing trend of case reports and case series publications. Most of these cases have been reported from South India, and few sporadic cases have been reported from the Eastern and Western regions.[4] To the best of our knowledge, this is the first report from the Uttarakhand region. With improvements in laboratory, detection and reporting the increase in sporadic cases suggests that the disease has spread beyond the tropics and subtropics and gaining the status of an emerging infectious disease.[5]
The common risk factors associated with this disease are diabetes, immunosuppression, alcoholism, and chronic infections. In India, up to 80% of melioidosis cases are diabetic.[4] In the present case, the patient was nondiabetic and had no history of any chronic disease. Among deep abscesses caused by B. pseudomallei, the spleen and liver are common sites of presentation.[3] In our case, the abscess was found in the liver.
Clinical diagnosis is usually missed due to a lack of awareness of the disease and a low index of suspicion among clinicians. As colonies of B. pseudomallei often appear wrinkled, it is assumed to be environmental, aerobic spore-bearing contaminants and is usually discarded.
CONCLUSIONS
In the present study, early identification of organisms helped clinicians initiate appropriate management. Since this was the first case in our area, we conducted a seminar on melioidosis to increase awareness among clinicians about this disease and adherence to long-term eradication treatment regimens following discharge from the hospital.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Liver abscess in children-clinical profile and outcome in a resource-limited setting. J Family Med Prim Care. 2022;11:7289-93.
- [CrossRef] [Google Scholar]
- Liver abscess caused by Burkholderia pseudomallei in a young man: A case report and review of literature. World J Clin Cases. 2014;2:604-7.
- [CrossRef] [Google Scholar]
- Melioidosis in a tertiary care center from South India: A 5-year experience. Indian J Crit Care Med. 2021;25:327-30.
- [CrossRef] [Google Scholar]
- Burden of melioidosis in India and South Asia: Challenges and ways forward. Lancet Reg Health Southeast Asia. 2022;2:100004.
- [CrossRef] [Google Scholar]
- Serodiagnosis of abdominal abscess caused by Burkholderia pseudomallei Case report and literature review. Infect Drug Resist. 2023;16:5613-25.
- [CrossRef] [Google Scholar]






