Translate this page into:
A Study on the Prevalence of Genital Trichomoniasis among Female Outpatients Attending Sexually Transmitted Infection Clinic in a Tertiary Care Hospital
Address for correspondence: Dr. Swapna Muthusamy, E-mail: swapnamuthuswamy@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Women with high-risk sexual behavior accounts for more than half of the sexually transmitted infection (STI) clinic attendees. The prevalence of trichomoniasis is as low as 5% in the general population to as high as 60% in high-risk population. This infection can pave the way to the acquisition of human immunodeficiency virus and other STIs, vice versa and is even associated with cancer.
Objectives:
To identify, isolate and study the prevalence of Trichomonas vaginalis in genital specimens of female outpatients.
Materials and Methods:
Total number of subjects involved in the study was 130, among them 85 belonged to high-risk group and 45 belonged to low-risk group. Two high vaginal swabs were collected from each patient. Saline wet mount, Giemsa stain, and culture in modified cysteine peptone liver infusion maltose medium were performed. Results were tabulated and analyzed.
Results:
Saline wet mount was positive for trichomoniasis in seven individuals, Giemsa detected trichomoniasis in five patients, and culture was positive in eight patients. Of these eight culture positive cases, one was wet mount negative and four were Giemsa stain negative.
Conclusion:
Culture is more sensitive than wet mount and Giemsa stain.
Keywords
Cysteine peptone liver infusion maltose medium
high-risk females
Trichomonas vaginalis
INTRODUCTION
Trichomoniasis is one of the neglected parasitic diseases that demands attention. This protozoal sexually transmitted disease is estimated to have a global prevalence of 8.1% among women and 1.0% among men.[1] In Indian scenario, the prevalence of trichomoniasis is about 6–10%.[2] Trichomoniasis is usually asymptomatic in males. Infected females may present with symptoms such as frothy, foul smelling green or yellow colored vaginal discharge, pruritus, dysuria, dyspareunia or lower abdominal pain, and 30% can be even asymptomatic.[3] Diagnostic methods available for trichomoniasis are wet mount preparation, staining methods, culture in laboratory medium, cell culture, and molecular methods. Adverse outcomes of trichomoniasis include perinatal morbidities such as preterm labor, premature rupture of membranes, low birth weight infant and infertility, cervical cancer, increased acquisition of human immunodeficiency virus (HIV), and other sexually transmitted infections (STIs).[456] Since high-risk females form one of the target groups for the prevention of STI transmission in the community, this study has been carried out to detect the prevalence of trichomoniasis among female outpatients focusing mainly on high-risk group.
MATERIALS AND METHODS
Our study included one hundred and thirty female outpatients categorized into two groups, namely high-risk group and low-risk group. High-risk group included female sex workers and females with multiple sexual partner and low-risk group included females with a single partner. Females with symptoms suggestive of trichomoniasis such as vaginal discharge, dyspareunia, burning micturition, pruritus, or lower abdominal pain were included in the study. Women in menstruation, genital prolapse, or with a history of treatment for discharge syndrome within 2 weeks prior to the visit were excluded from the study. This study was done over a period of 1 year extending from February 2012 to January 2013. Ethical and research clearance were obtained from the Institutional Ethical and Research Committee, Stanley Medical College. Informed consent was obtained from each patient before enrollment into the study. The procedure was explained to the patient and two high vaginal swabs were collected from each individual. Discharge from speculum was used for preparing saline mount, one high vaginal swab was used for Giemsa stain and another high vaginal swab was inoculated into modified cysteine peptone liver infusion maltose (CPLM) medium for culture.
The presence of Trichomonas vaginalis was determined by pear-shaped motile trophozoites in wet mount. Giemsa stain was performed to look for the pear-shaped morphology of T. vaginalis. Modified CPLM medium after inoculation was incubated in CO2atmosphere for 1 week, and wet mount was performed from the medium every day to look for motile trophozoites.
Patients were also tested for HIV and syphilis. They were advised to visit Integrated Counselling and Testing Centre room where pretest counseling was given before sample collection. Samples were tested for HIV following national guidelines. Samples which were nonreactive by the first test (Comb AIDS) were reported as such and reactive samples were subjected to the second (SD Bioline HIV 1/2) and third test (HIV Tridot). Results were informed to the patients after posttest counseling. Reactive patients were advised to visit antiretroviral therapy clinic for further follow-up and treatment. Syphilis was tested using rapid plasma regain (RPR) card test.
RESULTS
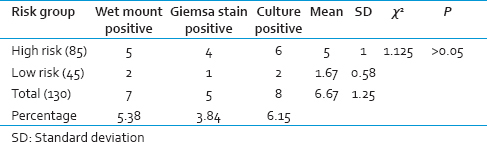
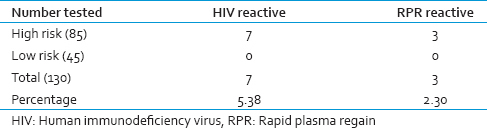
A total number of females involved in our study was 130, of whom 85 belonged to high-risk group and 45 belonged to low-risk group. Vaginal discharge samples collected from them were subjected to wet mount, Giemsa stain, and culture. Results were tabulated and analyzed for percentage, mean, standard deviation, and P value. The number of female patients positive for trichomoniasis by wet mount, Giemsa stain, and culture were 5, 4, and 6 in high-risk group and 2, 1, and 2 in low-risk group, respectively. The detection of positivity by culture was more compared to wet mount and Giemsa stain. Even though the differences in the detection of positives by three methods did not show statistical significance, culture detected one case which was both wet mount and Giemsa stain negative. The mean positivity of trichomoniasis among high-risk and low-risk groups was 5 and 1.67, respectively [Table 1]. HIV and RPR reactivity in our study were 5.38% and 2.30%, respectively, which were exclusively seen in high-risk group [Table 2].
DISCUSSION
The World Health Organization has reported that trichomoniasis accounts for almost half of all curable STIs. Vaginal discharge is often treated based on the clinical evaluation. Characteristic features of trichomoniasis like frothy discharge and strawberry cervix are appreciable in minimal percentage (10% and 2%) of infected females only. If patients are treated based on clinical diagnosis alone, majority of infected women will go untreated, and few of uninfected women may even get treated unnecessarily. Therefore, it is essential to diagnose trichomoniasis using microbiological tests.
Wet mount is a simple microscopic test that needs a minimal concentration of 104 organisms/ml of vaginal secretion. However, it is essential to perform microscopy within 10 min of sample collection after which efficacy of the test decreases.[7] Stains that can be used for trichomoniasis are Giemsa stain, acridine orange, Leishman's stain, periodic acid-Schiff, and Fontana stain. Culture is the gold standard for diagnosis of trichomoniasis. It can pick up positivity if 300–500 organisms/ml are present in the specimen. Media available for cultivation of T. vaginalis are Diamond's/modified Diamond's medium, CPLM/modified CPLM medium, Feinberg Whittington medium, Lash medium, Kupferberg medium, agar culture, and InPouch TV culture. Saksirisampant et al. have compared CPLM, modified CPLM, and BBL media and found that modified CPLM is the cost effective media for culture of T. vaginalis.[8] In our study, we have performed wet mount, Giemsa stain, and culture using modified CPLM medium.
The subjects in our study belonged to reproductive age group (15–49 years). Among the participants, 50% of individuals belonged to 30–39 years age decade. T. vaginalis positives were detected more among females belonging to 20–29 years age decade followed by 30–39 years. The study by Donbraye et al. showed that 63% of their study subjects belonged to 20–29 years of age and most common age decade that showed T. vaginalis positivity is <20 years.[9] The study done by Jatau et al. showed that T. vaginalis infection is more prevalent among 16–25 years age group followed by 26–35 years age group.[10]
The prevalence of trichomoniasis in our study was 6.15% with high-risk group showing a higher prevalence of 7.05% and low-risk group showing 4.44% prevalence. In a study done by Deivam et al. in a rural tertiary care hospital, the prevalence of trichomoniasis was found to be 8.1%.[11] In another study conducted by Das et al. among female sex workers in Mumbai and Hyderabad, the prevalence was 29.73%.[12] Das et al. study demonstrated a very high prevalence of trichomoniasis, probably because the study was carried out among commercial sex workers in known high prevalent areas. According to Donbraye et al., the incidence of trichomoniasis is the highest in women with multiple partners.[9] Our study also showed that the prevalence of trichomoniasis was more in high-risk group compared to low-risk group.
In our study, culture (6.15%) identified more cases than wet mount (5.38%) and Giemsa stain (3.84%) [Table 1]. Order of sensitivity of three methods in our study correlates well with the findings of the study done by Akujobi et al. where culture (9.04%) was more sensitive than wet mount (8.01%) and Giemsa stain (6.71%).[13] However, the percentage positivity was slightly lower in our study compared to Akujobi et al. study.
Tests for HIV and RPR in our study showed that percentage of reactive samples was 5.38 and 2.30, respectively. Detection of HIV in patients with trichomoniasis is important because of the common mode of transmission and also due to the reason that any STI increases the acquisition and transmission of HIV and vice versa. In the study done by Mavedzenge et al., they found an increased risk of HIV acquisition among trichomoniasis patients and increased T. vaginalis acquisition among HIV-infected individuals.[6] A study by Hutton-Rose et al. have shown that the prevalence of trichomoniasis in HIV reactive individuals was 15%.[14]
Wet mount positive individuals were given metronidazole on the day of visit and one patient who was wet mount and Giemsa stain negative, but culture positive was also treated during the follow-up visit.
Limitation of our study is that contact tracing is an important aspect in the control of any STIs but was not successful in our study due to the reason that majority of our study population were sex workers who were not willing to bring their partners. List of reasons narrated by sex workers for unsuccessful contact tracing was a practical difficulty in bringing multiple partners, fear of losing their source of income, unwilling to reveal their partners' identity, fear of patient's identity being exposed by partners, and professional ethics.
CONCLUSION
The prevalence of trichomoniasis was higher in high-risk group than low-risk group. The culture was more sensitive than wet mount and Giemsa stain. In resource-poor settings, wet mount is a good option for diagnosing trichomoniasis but wherever facilities are available culture should be performed to identify wet mount negative cases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Global Prevalence and Incidence of Selected Curable Sexually Transmitted Infections: Overview and Estimates. Geneva, Switzerland: World Health Organization (WHO); 2001.
- Trichomoniasis among women in north India: A hospital based study. Indian J Sex Transm Dis. 2008;29:76-81.
- [Google Scholar]
- The prevalence of trichomoniasis in high-risk behavior women attending the clinics of Tehran province penitentiaries. Iran J Med Sci. 2010;35:190-4.
- [Google Scholar]
- Trichomonas vaginalis as a cause of perinatal morbidity: A systematic review and meta-analysis. Sex Transm Dis. 2014;41:369-76.
- [Google Scholar]
- Epidemiological synergy of Trichomonas vaginalis and HIV in Zimbabwean and South African women. Sex Transm Dis. 2010;37:460-6.
- [Google Scholar]
- Clinical and laboratory evidence of Trichomonas vaginalis infection among women of reproductive age in rural area. Indian J Med Microbiol. 2012;30:314-6.
- [Google Scholar]
- Cost identification analysis of culture methods for trichomoniasis. Arch Hell Med. 2009;26:517-9.
- [Google Scholar]
- Detection and prevalence of Trichomonas vaginalis among pregnant women in Ibadan, Southwestern Nigeria. World Appl Sci J. 2010;11:1512-7.
- [Google Scholar]
- Prevalence of Trichomonas vaginalis infection among women attending antenatal clinics in Zaria, Nigeria. Ann Afr Med. 2006;5:178-81.
- [Google Scholar]
- Prevalence of Trichomonas vaginalis infection among patients that presented to rural tertiary care hospital in Tiruchirappalli, India in 2011 and 2013. Int J Pharm Res Health Sci. 2014;2:255-60.
- [Google Scholar]
- Prevalence and assessment of clinical management of sexually transmitted infections among female sex workers in two cities of India. Infect Dis Obstet Gynecol. 2011;2011:494769.
- [Google Scholar]
- Comparison of saline wet preparation, Giemsa staining and culture methods for the detection of Trichomonas vaginalis. Afr J Clin Exp Microbiol. 2006;7:208-11.
- [Google Scholar]
- The prevalence of other sexually transmitted infections in confirmed HIV cases at a referral clinic in Jamaica. J R Soc Promot Health. 2008;128:242-7.
- [Google Scholar]





