Translate this page into:
Association of Secondary Hyperparathyroidism with Hemoglobin Level in Patients with Chronic Kidney Disease
Address for correspondence: Dr. Happy Chutia, E-mail: happy.chutia@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
How to cite this article: Chutia H, Ruram AA, Bhattacharyya H, Boruah P, Nath C. Association of secondary hyperparathyroidism with hemoglobin level in patients with chronic kidney disease. J Lab Physicians 2013;5:51-4.
Abstract
Purpose:
Secondary hyperparathyroidism (SHPT) is one of the less recognized reasons of anemia in chronic kidney disease (CKD). In this study, we evaluated the role of SHPT as a cause of anemia and correlation of intact parathyroid hormone (iPTH) and hemoglobin (Hb) level in hemodialysis (HD) patients.
Methods:
This cross-sectional study was carried out in 63 individuals admitted in HD unit of the institute. Serum samples were collected and urea, creatinine, Hb, ferritin and iPTH levels were measured. Statistical analysis was carried out using the SPSS software (IBM, NY, USA).
Results:
Mean ± standard deviation for serum urea, creatinine, Hb, ferritin and intact PTH were 177 ± 15.52, 15.16 ± 2.28 mg/dl, 7.03 ± 2.26 g/dl, 654.7 ± 563.4 ng/ml, 539.18 ± 493.59 pg/ml respectively. A reverse correlation was found between intact PTH and Hb level.
Conclusions:
A variety of postulated pathophysiological mechanisms linking SHPT and anemia in CKD are discussed. An efficient control of parathyroid hormone hypersecretion may be required to achieve a better management of anemia in HD patients.
Keywords
Anemia
chronic kidney disease
ferritin
hemoglobin
intact parathyroid hormone
secondary hyperparathyroidism
INTRODUCTION
Chronic kidney disease (CKD) is defined as functional abnormalities of the kidney lasting longer than 3 months, with or without reduced glomerular filtration rate. It can also be defined by the presence of urinary albumin with an excretion rate higher than 300 mg/24 h or in a ratio of more than 200 mg of albumin to 1 g of creatinine.[1] The prevalence of CKD, in India ranges from 0.79% to 1.4%.[2]
Hyperparathyroidism secondary to CKD is an overproduction of parathyroid hormone (PTH) caused by several changes that occur in bone and mineral metabolism as a result of decreased kidney function. The first change that usually occurs with declining kidney function involves the deficiency of activated vitamin D and an increase in phosphorus excretion by the remaining functional nephrons. Both of these changes stimulate an increase in PTH synthesis and secretion. Secondary hyperparathyroidism (SHPT) develops early in the course of the disease before dialysis initiation. Unfortunately, it is often unrecognized and inadequately treated in patients with early stages of kidney disease when therapy would have greater benefits.
Anemia has been recognized as a possible complication of primary hyperparathyroidism.[3] Since hyperparathyroidism can induce anemia in patients with normal kidney function, SHPT due to CKD may also have an unfavorable influence on anemia of uremic patients. There is also indirect evidence of restoration of the hematocrit after parathyroidectomy in uremic patients due to restoration of bone marrow space after operation and rise of immunoreactive erythropoietin (EPO) serum concentrations.[4]
Factors that may be responsible for anemia in CKD are blood loss, shortened red cell life span, vitamin deficiencies, EPO deficiency, iron deficiency, infection and inflammation. Among these, EPO deficiency is considered as the most important cause.[5] The introduction of recombinant human erythropoietin (rhEPO) therapy in the early 1990s for treatment of anemia of patients undergoing hemodialysis (HD) has led to a significant reduction in anemia and to an improvement in patients' quality-of-life.[5] However, there is a significant variability among HD patients in the sensitivity to rhEPO. Moreover, around 5-10% of the patients show a marked resistance to rhEPO therapy.[6-10] The European Best Practice Guidelines define “resistance to rhEPO therapy” as a failure to achieve target hemoglobin (Hb) levels (between 11 and 12 g/dl) with maintained doses of rhEPO.[6] There are many causes of this variability of resistance to rhEPO therapy. One of the possible reasons may be SHPT. Hemodialysis patients with SHPT, usually associated with osteitis fibrosa on bone histology, show considerable resistance to EPO, which is partly because of replacement of the bone marrow by fibrous tissue.
In this study, we have analyzed the effect of SHPT in aggravating the anemia and correlation of intact parathyroid hormone (iPTH) and Hb level if there is any, in HD patients.
MATERIALS AND METHODS
This cross-sectional study was carried out in 63 patients admitted in HD unit of North East Indira Gandhi Institute of Health and Medical Science. Serum urea, creatinine, Hb, ferritin and intact PTH were measured. Patients taking angiotensin-converting enzyme-inhibitors, non-steroidal anti-inflammatory drugs and those having external blood loss were excluded. Baseline data of patients like age and sex were recorded. Institutional review was not necessary as it was a retrospective study.
All blood specimens were drawn as pre-dialysis. Blood chemistry analysis was carried out with the Beckman coulter auto-analyzer AU2700. Serum ferritin and intact PTH were assayed by chemiluminescence method (Access2, Beckman coulter).
A database was constructed on Microsoft Excel 2007 and statistical analyses were performed using the SPSS software version 20.0 (IBM, NY, USA).
RESULTS
In our study, comprising 63 patients 31 (49.2%) were men and 32 (50.8%) were women with nearly equal sex distribution. 17 patients (27.0%) were in the age group 20-40 years, 33 (52.4%) were in the age group 40-60 years and 13 (20.6%) were in the age group 60-80 years. Mean ± standard deviation for serum urea, creatinine, Hb, ferritin and iPTH were 177 ± 15.52 mg/dl, 15.16 ± 2.28 mg/dl, 7.03 ± 2.26 g/dl, 654.7 ± 563.4 ng/ml, 539.18 ± 493.59 pg/ml respectively.
Three patients (4.8%) had normal iPTH levels (12-88 pg/ml) and rest of patients had raised levels of iPTH (95.2%). With respect to ferritin, 23 (36.5%) had normal ferritin level of 11-336 ng/ml; 40 (63.5%) had a raised levels of ferritin. All patients had Hb level of <13 g/dl.
No significant association was observed between age and iPTH (Chi-square = 6.967, df = 4), age and Hb levels (Chi-square = 2.027, df = 6, P > 0.05) and between age and ferritin levels. (Chi-square = 8.361, df = 4, P > 0.05). Furthermore, no significant association was observed between ferritin and iPTH levels. (Chi-square = 4.550, df = 4, P > 0.05) and ferritin and Hb levels (Chi-square = 4.766, df = 6, P > 0.05). A significant association was however observed between PTH and Hb levels (Chi-square = 26.942, df = 6, P < 0.001).
Similarly, bivariate analysis was carried out including serum PTH, Hb, Age and ferritin did not show any relationship between these parameters except Hb and PTH i.e., a Pearson's correlation of −0.545 and covariance −0.609.3, which were statistically significant.
A reverse correlation was found between intact PTH and Hb level (r = −0.545), which indicates that the variables iPTH and Hb level are inversely proportional to each other [Figure 1]. More importantly, no correlation was observed between iPTH and ferritin (r = 0.0709) indicating that anemia is not due to depleted iron stores.
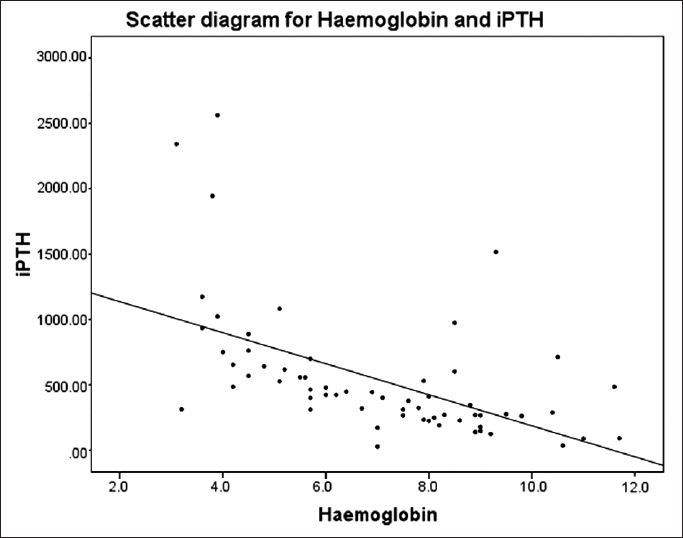
- Scatter diagram showing reverse correlation between iPTH and Hb level in CKD patients
DISCUSSION
The development of SHPT as well as anemia is a common complication of CKD. The World Health Organization has defined anemia as an Hb concentration lower than 13.0 g/dl in men and post-menopausal women and less than 12.0 g/dl in other women. In this study, a significant association was found between PTH and Hb level, which is consistent with the findings of Baradaran and Nasri, [11] Sliem et al.[12] and Trovato et al.[13] A reverse correlation was found between PTH and Hb level. Possible causes of low Hb level or anemia due to SHPT may be because of increased bone marrow fibrosis, which may lead to decreased erythropoietin and increased resistance to EPO.[14] Erythropoietin cells express calcitriol receptors, which induces proliferation and maturation of erythroid progenitor cells. Therefore, deficiency of calcitriol, a cause of hyperparathyroidism may impair erythropoiesis. There are also some studies, which support an increase in erythrocyte osmotic fragility due to high concentration of PTH in patients on dialysis, leading to low Hb level.[15]
Management of SHPT is a challenge frequently encountered in the patients with CKD. Down-regulation of the parathyroid vitamin D and calcium-sensing receptors are the critical steps that lead to abnormalities in mineral metabolism: High phosphate, low calcium and vitamin D deficiency. These imbalances result in parathyroid hyperplasia leading to SHPT and elevated serum calcium, phosphorus, calcium-phosphorus product. As a result of these, relative risk of mortality increases.[16]
An efficient control of PTH hypersecretion is therefore required to achieve a better management of anemia as well as mineral metabolism in HD patients.
The medical management of SHPT in patients with CKD principally involves dietary changes, the use of the combination of phosphate binders, active vitamin D analogs and/or calcimimetics (which increase the sensitivity of the calcium sensing receptors to calcium).[16] In addition, they need treatment of underlying conditions including hypertension, cardiac ailments and diabetes.
Patients with CKD need special diet with restriction of salt, potassium, phosphorous and other electrolytes. Protein restriction while getting enough calories to prevent weight loss is also needed. However, dietary recommendations may change over time as patient's disease progresses. For example, during dialysis protein requirement increases hence patient needs extra proteins. Calcium supplementation is necessary to prevent loss of calcium from bones; however, dairy products must be avoided they also contain high amount of phosphorus. Restricting fluids, common salt and fruits containing high potassium is also needed to maintain adequate fluid and electrolyte balance. Patient also needs extra iron to prevent anemia, which can occur because of various reasons already mentioned.[17-20]
More wider and detailed studies are necessary to confirm the findings and to explain the mechanisms underlying the improvement in anemia after medical or surgical treatment of SHPT.
Source of Support:
Nil.
Conflict of Interest:
None declared.
ACKNOWLEDGMENTS
We are thankful to the patients for their participation and to the team of biochemistry and pathology laboratories for their help. We are also thankful to the hemodialysis unit of the institute for their support. Dr. Akash Handique provided us helpful feedback on the manuscript.
REFERENCES
- K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(Suppl 1):S1-266.
- [Google Scholar]
- Burden of disease-Prevalence and incidence of renal disease in India. Clin Nephrol. 2010;74(Suppl 1):S9-12.
- [CrossRef] [PubMed] [Google Scholar]
- Anemia and secondary hyperparathyroidism. Arch Intern Med. 1978;138:1650-2.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of secondary hyperparathyroidism in chronic kidney disease and the direct costs of treatment. J Manag Care Pharm. 2007;13:397-411.
- [CrossRef] [PubMed] [Google Scholar]
- Anemia in chronic kidney disease: Causes, diagnosis, treatment. Cleve Clin J Med. 2006;73:289-97.
- [CrossRef] [PubMed] [Google Scholar]
- Resistance to recombinant human erythropoietin therapy in hemodialysis patients- Focus on inflammatory cytokines, leukocyte activation, iron status and erythrocyte damage. J Nephrol Ren Transplant. 2009;2:66-83.
- [Google Scholar]
- Inflammation, serum C-reactive protein, and erythropoietin resistance. Nephrol Dial Transplant. 2001;16:224-7.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammation and resistance to erythropoiesis-stimulating agents - What do we know and what needs to be clarified? Nephrol Dial Transplant. 2005;20(Suppl 8):viii,2-7.
- [CrossRef] [PubMed] [Google Scholar]
- Erythropoietin resistance: The role of inflammation and pro-inflammatory cytokines. Nephrol Dial Transplant. 2002;17(Suppl 11):39-43.
- [CrossRef] [PubMed] [Google Scholar]
- Influencing the inflammatory response of haemodialysis patients by cytokine elimination using large-pore membranes. Nephrol Dial Transplant. 2002;17:17-9.
- [CrossRef] [PubMed] [Google Scholar]
- Intensification of anaemia by secondary hyperparathyroidism in hemodialysis patients. Med J Islam Acad Sci. 2001;14(4):161-6.
- [Google Scholar]
- Relationship of associated secondary hyperparathyroidism to serum fibroblast growth factor-23 in end stage renal disease: A case-control study. Indian J Endocrinol Metab. 2011;15:105-9.
- [CrossRef] [PubMed] [Google Scholar]
- Hyperparathyroidism, anaemia and erythropoietin: Effects on systolic function of dialysis patients. Abstracts of 31st Congress of European Renal Association/European dialysis ND Transplantation Association, September 5-8, 1999, Madrid in Nephrol Dial. Transpl. 1999;14:190.
- [Google Scholar]
- Hyperparathyroidism and anemia in renal failure. Am J Nephrol. 2000;20:89-96.
- [CrossRef] [PubMed] [Google Scholar]
- Red blood cell osmotic fragility in chronically hemodialyzed patients. Nephron. 1998;78:28-32.
- [CrossRef] [PubMed] [Google Scholar]
- Secondary hyperparathyroidism: Pathogenesis, disease progression, and therapeutic options. Clin J Am Soc Nephrol. 2011;6:913-21.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical practice. Stage IV chronic kidney disease. N Engl J Med. 2010;362:56-65.
- [CrossRef] [PubMed] [Google Scholar]
- Dietary Guidelines for Adults Starting on Hemodialysis, 2010. National Kidney Foundation. Available from: http://www.kidney.org/atoz/pdf/nutri_hemo.pdf (accessed )
- [Google Scholar]
- NIH Publication. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK. Weblink: Available from: http://kidney.niddk.nih.gov/kudiseases/pubs/eatright/ (accessed )
- [Google Scholar]
- Rapid Update 2011. NICE Clinical Guidelines, No. 114 National Clinical Guideline Centre (UK) London: Royal College of Physicians (UK); 2011. weblink: Available from: http://www.ncbi.nlm.nih.gov/books/NBK65527/ (accessed )
- [Google Scholar]





