Translate this page into:
Biomedical waste management in India: Critical appraisal
Address for correspondence: Dr. Priya Datta, Department of Microbiology, Government Medical College Hospital, Sector 32, Chandigarh - 160 030, India. E-mail: drpriyadatta@hotmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The safe and sustainable management of biomedical waste (BMW) is social and legal responsibility of all people supporting and financing health-care activities. Effective BMW management (BMWM) is mandatory for healthy humans and cleaner environment. This article reviews the recent 2016 BMWM rules, practical problems for its effective implementation, the major drawback of conventional techniques, and the latest eco-friendly methods for BMW disposal. The new rules are meant to improve the segregation, transportation, and disposal methods, to decrease environmental pollution so as to change the dynamic of BMW disposal and treatment in India. For effective disposal of BMWM, there should be a collective teamwork with committed government support in terms of finance and infrastructure development, dedicated health-care workers and health-care facilities, continuous monitoring of BMW practices, tough legislature, and strong regulatory bodies. The basic principle of BMWM is segregation at source and waste reduction. Besides, a lot of research and development need to be in the field of developing environmental friendly medical devices and BMW disposal systems for a greener and cleaner environment.
Keywords
2016
Biomedical waste
changes
India
Introduction
Biomedical waste (BMW) is any waste produced during the diagnosis, treatment, or immunization of human or animal research activities pertaining thereto or in the production or testing of biological or in health camps. It follows the cradle to grave approach which is characterization, quantification, segregation, storage, transport, and treatment of BMW.
The basic principle of good BMW practice is based on the concept of 3Rs, namely, reduce, recycle, and reuse. The best BMW management (BMWM) methods aim at avoiding generation of waste or recovering as much as waste as possible, rather than disposing. Therefore, the various methods of BMW disposal, according to their desirability, are prevent, reduce, reuse, recycle, recover, treat, and lastly dispose. Hence, the waste should be tackled at source rather than “end of pipe approach.”[1]
BMW treatment and disposal facility means any facility wherein treatment, disposal of BMW or processes incidental to such treatment and disposal is carried out.[1]
Only about 10%–25% of BMW is hazardous, and the remaining 75%–95% is nonhazardous. The hazardous part of the waste presents physical, chemical, and/or microbiological risk to the general population and health-care workers associated with handling, treatment, and disposal of waste.[2]
In a World Health Organization (WHO) meeting in Geneva, in June 2007, core principles for achieving safe and sustainable management of health-care waste were developed. It was stressed that through right investment of resources and complete commitment, the harmful effects of health-care waste to the people and environment can be reduced. All stakeholders associated with financing and supporting health-care activities are morally and legally obliged to ensure the safety of others and therefore should share in the cost of proper management of BMW. In addition, it is the duty of manufacturer to produce environment-friendly medical devices to ensure its safe disposal. WHO reinforced that government should designate a part of the budget for creation, support, and maintenance of efficient health-care waste management system. These include novel and ingenious methods/devices to reduce the bulk and toxicity of health-care waste. Nongovernmental Organization should undertake program and activities that contribute in this incentive.[3]
The first edition of WHO handbook on safe management of wastes from health-care activities known as “The Blue Book” came out in 1999. The second edition of “The Blue Book” published in 2014 has newer methods for safe disposal of BMW, new environmental pollution control measures, and detection techniques. In addition, new topics such as health-care waste management in emergencies, emerging pandemics, drug-resistant bacteria, and climate changes were covered in the second edition.[1]
International Agreement and Conventions
There are three international agreements and conventions which are particularly pertinent in BMWM, environment protection, and its sustainable development and therefore should be kept in mind by preparing waste management policies. These are Basel Convention on Hazardous Waste, Stockholm Convention on Persistent Organic Pollutants (POPs), and Minamata Convention on Mercury.
Basel Convention on Hazardous Waste is the most inclusive global environmental treaty on hazardous and other wastes. It has 170 member countries, and its objectives are to protect human health and the environment against the adverse effects resulting from the generation, management, and disposal of hazardous wastes, specifically clinical wastes from health care in hospitals, health centers, and clinics.[4]
Stockholm Convention on POPs (the Stockholm Convention) is a global treaty to protect human health and the environment from POPs (POPs – dioxins and furans). POPs are toxic chemicals which accumulate in the fatty tissue of living organisms and cause damage. These chemicals are formed by medical waste incinerators and other combustion processes. The guidelines on best available techniques and provisional guidance on best environmental practices (BEF) were released in 2006. It deals with BEP including source reduction, segregation, resource recovery and recycling, training, and proper collection and transport.[5]
Minamata Convention on Mercury is a global treaty to protect human health and the environment from the adverse effects of mercury. On October 10, 2014, in Japan, more than 90 nations signed the first new global convention on environment and health. This treaty includes the phasing out of certain medical equipment in health-care services, including mercury-containing medical items such as thermometers and blood pressure device.[6]
Biomedical Waste Management Outside India
In 2012, WHO conducted a survey on the BMWM status of 24 countries of West Pacific area, which included countries such as Japan, China, Australia, New Zealand, Philippines, Malaysia, Vietnam, Cambodia, Republic of Korea, Micronesia, Nauru, and Kiribati. The survey included a literature search, review of publications, newspaper articles, and other sources of information. The status in each country was assessed on five main areas of BMW, namely, management, training, policy and regulatory framework, technologies implemented, and financial resources. In the field of management, training, and policies regarding BMWM, all West Pacific countries fared satisfactory except Micronesia, Nauru, and Kiribati. Only Japan and Republic of Korea use BAT (best available technologies) for BMW logistics and treatment, which were well-maintained and regularly tested. Most of the countries had no or very less financial resources for BMWM. Therefore, HCWM is still far from ideal in most of West Pacific countries, and additional backing for the expansion of HCWM systems in countries is vital to ensure that within the next decade, safe HCWM systems are applied.[7]
In Canada, there is variation seen in the medical waste – management practices across different provinces. Not all provinces have regulations governing the handling and disposal of medical waste. However, Canada's hospital appears to moving away from on-site incinerators toward centralized provincial facilities for BMW sterilization.[8]
Biomedical Waste Situation in India
In July 1998, first BMW rules were notified by Government of India, by the erstwhile Ministry of Environment and forest.[9] In India, BMW problem was further compounded by the presence of scavengers who sort out open, unprotected health-care waste with no gloves, masks, or shoes for recycling, and second, reuse of syringe without appropriate sterilization.[3]
During 2002–2004, International Clinical Epidemiology Network explored the existing BMW practices, setup, and framework in primary, secondary, and tertiary health care facility (HCF) in India across 20 states.[10] They found that around 82% of primary, 60% of secondary, and 54% of tertiary HCFs in India had no credible BMWM system. In 2009, around 240 people in Gujarat, India contracted hepatitis B following reuse of unsterilized syringes.[11] This and many more studies shows that despite India being among the first country to initiate measures for safe disposal of BMW, there is an urgent need to take action for strengthening the existing system capacity, increase the funding and commitment toward safe disposal of BMW.
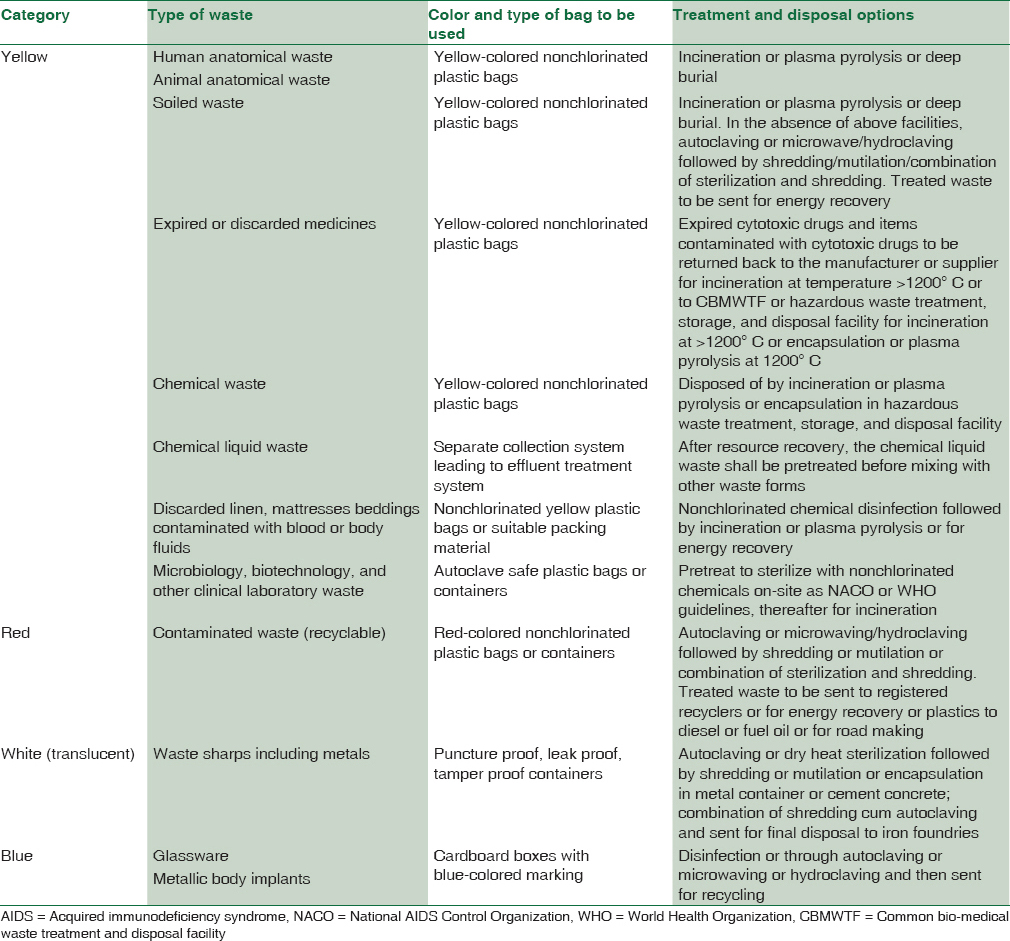
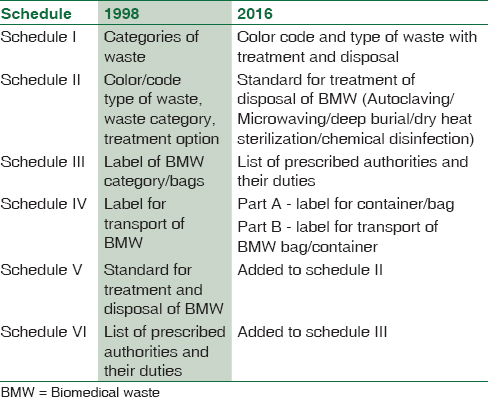
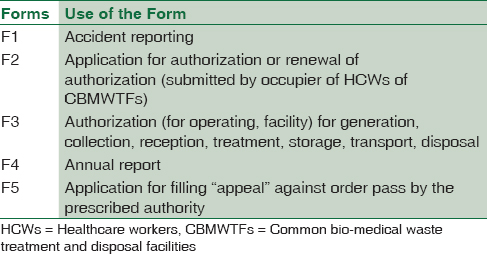
The BMW 1998 rules were modified in the following years – 2000, 2003, and 2011. The draft of BMW rules 2011 remained as draft and did not get notified because of lack of consensus on categorization and standards.[12] Now Ministry of Environment, Forest and Climate change in March 2016 have amended the BMWM rules [Table 1]. These new rules have increased the coverage, simplified the categorization and authorization while improving the segregation, transportation and disposal methods to decrease environmental pollution [Table 2]. It has four schedule, five forms and eighteen rules [Tables 3 and 4].[13]

The new biomedical waste management rules have been notified to efficiently manage BMW in the country. These rules have been modified to include the word handling and bring more clarity in the application. In addition, strict rules have been made to ensure no pilferage of recyclables item, no secondary handling or in advent scattering or spillage by animals during transport from the HCFs to the common BMW treatment facility (CBMWTF). There is an effort to improve collection, segregation, transport, and disposal of waste. Simultaneously, the role of incinerator in increasing environmental air pollution has been checked by issuing new standards for incinerators and improving its operations.[13]
Data from Government of India site indicates the total BMW generated in the country is 484 TPD (tonnes per day) from 1, 68,869 HCFs. Unfortunately, only 447 TPD is treated, and 37 TPD is left untreated. There are 198 CBMWTF in operation and 28 under construction. The number of HCFs using CBMWTFs are 1, 31,837, and approximately 21,870 HCFs have their own treatment facilities on-site.[13]
As per the BMW Rules, 1998, and as amended, any HCF or CBWTF operator wanting to use other innovative and improved technologies other than stipulated under Schedule-I of the Rules, shall approach the Central Pollution Control Board (CPCB) to get the standards laid down to enable the prescribed authority to consider grant of authorization. During the year 2010–2013, CPCB have granted conditional or provisional approval to new technologies (other than notified under BMW Rules) for treatment of BMW. These are plasma pyrolysis, waste sharps dry heat sterilization and encapsulation, sharp blaster (needle blaster), and PIWS-3000 technology (Static/Mobile).
Salient Features of Biomedical Waste Rules 2016
-
The scope of the rules have been expanded to include various health camps such as vaccination camps, blood donation camps, and surgical camps[13]
-
Duties of the occupier of a HCFs have been revised. Occupier is the person having administrative control over the HCF that is generating BMW[8]
-
Compulsory pretreatment of the laboratory, microbiological waste, and blood bags on-site before disposal either at CBMWTF or on-site. The method of sterilization/disinfection should be in accordance with National AIDS Control Organization (NACO) or WHO
-
The use of chlorinated plastic bags, gloves, blood bags, etc. should be gradually stopped and this phasing out should be within 2 years from the date of notification of these rules
-
To provide training to all its HCWs and protect them against diseases such as hepatitis B and tetanus by immunization
-
Liquid waste to be separated at source by pretreatment before mixing with other liquid waste
-
To set up a barcode system for BMW containing that is to be sent out of the premises for treatment and disposal
-
All major accidents including accidents caused by fire hazards, blasts, during handling of BMW, and remedial action taken by the prescribed authority should be reported
-
The existing incinerator should be upgraded/modified to achieve the new standard within 2 years from the date of this notification
-
BMW disposal register is to be maintained daily and updated monthly on the website.
-
-
The duties of the operator of a common biomedical waste treatment and disposal facility (CBMWTF) have been increased.[13] They should assist in training of HCW from where the waste is being collected. Furthermore, there should be barcoding and global positioning system established for handling of BMW within 1 year. Maintain all records for operation of incineration/hydroclaving/autoclaving for a period of 5 years
-
The segregation, packaging, transportation, and storage of BMW have been improved. Biomedical waste has been classified into four categories based on color code-type of waste and treatment options. In addition, untreated human anatomical waste, animal anatomical waste, soiled waste, and biotechnology waste should not be stored beyond a period of 48 h. In case, there is a need to store beyond 48 h, the occupier should take all appropriate measures to ensure that the waste does not adversely affect human health and the environment (no permission to be obtained)[13]
-
No HCF shall establish on-site BMW treatment and disposal facility if the provision of CBMWTF is present at a distance of seventy-five kilometers. If no CBMWTF is available, the occupier shall set up requisite BMW treatment facility such as incinerator, autoclave or microwave, shredder after taking prior authorization from the prescribed authority. After confirming treatment of plastics and glassware by autoclaving or microwaving followed by mutilation/shredding, these recyclables should be given to authorized recyclers
-
Authorization for BMW disposal for nonbedded HCFs is granted to the occupier at one time only. The validity of authorization shall be synchronized with validity of consent orders for bedded HCFs
-
Standards for emission from incinerators have been modified to be more environmental friendly. These are permissible limit for SPM-50 mg/nm3; residence time in secondary chamber of incinerator – two seconds; standard for dioxin and furans – 0.1 ng TEQ/Nm3
-
Ministry of Environment, Forest, and Climate change will monitor the implementation of rules yearly. The responsibility of each state to check for compliance will be done by setting up district-level committee under the chairpersonship of District Collector or District Magistrate or Additional District Magistrate. In addition, every 6 months, this committee shall submit its report to the State Pollution Control Board.
Benefits of the new biomedical waste rules
The new rules are stringent and elaborate and should bring about a change in the way, the BMW is being managed in India. Under the new rules, coverage has increased to include various health-care related camps such as vaccination camps, blood donation camps, and surgical camps.
Another distinction is in the segregation, packaging, transport, and storage of BMW waste. The categories have been reduced to four to bring about ease of segregation. One of the main principle of disposal of BMW is that segregation has to be done at the source of generation of the waste. To overcome confusion created by large number of categories, this has been simplified to make it convenient and manageable for all HCWs. Now, the color coding (i.e., yellow, red, white, and blue) of the bags/containers is linked to a particular type of waste and its specific treatment option. For example, the disposal of chemical solid waste and cytotoxic waste to be done in yellow bag which goes for incineration/plasma pyrolysis/deep burial.
In addition, the HCF has to do pretreatment of various laboratory waste and blood bags according to guidelines of WHO and NACO, to decrease chances of infections being transmitted to HCWs handling waste at treatment stage. Within 2 years, plastic bags, gloves, and blood bags have to be phased out to eliminate emissions of dioxins and furans during their burning into the environment. The new rule also calls for a bar code system for all bags/containers used for BMW treatment and disposal. This step will help in tracking and identifying bags during inspection for quality control and also quality assurance.
The BMW in red/blue bag or container which is for recycling will be sent only to an authorized recycler. This will keep the recycler in realm and in control of various government agencies. Greater emphasis has been given to recycling of waste to conserve resources as well as decrease pollution.
The 2016 guidelines are more specific regarding the dependence of HCFs on CBMWTF and who will provide land for setting up CBMWTF. State government or UT government will provide land for setting up CBMWTF and no occupier of an HCF shall establish an on-site treatment and disposal facility if a CBMWTF is available within 75 kms. This has several advantages as installation and functioning of individual BMW treatment facility as well as recruiting separate, dedicate, and skilled workforce require high capital investment. CBMWTF is a popular concept in developed countries because by operating it at its full potential, the cost of treatment/kg BMW gets significantly reduced. Further, this makes control and checking of various waste disposal plants less tedious. Furthermore, maintaining records and log book will streamline the documentation.
The emission standards for incinerator has been made more stringent (acceptable SPM reduced to 50 mg/nm3, retention time in secondary camber lowered to 2 s). This will reduce dioxins and furans release (which are produced at temperature greater than 600°C) and lead to production of carbon dioxide and water.
The new rules lays down new criteria for authorization of an HCF and have made the procedure for getting authorization very simple. Bedded hospitals will get automatic authorization and nonbedded HCFs will get a one-time authorization.
Another improvement in the new rules is in the monitoring sector. The MoEF (Ministry of Environment, Forest, and Climate change) will review HCFs once a year through state health secretaries and the SPCB (State Pollution Control Board). Moreover, according to the new rules, the advisory committee on BMWM is now mandated to meet every 6 months.
Challenges in the Implementation of New Biomedical Waste 2016 Rules
One of the biggest challenges the government hospitals and small HCFs will face, during the implementation of BMW 2016 rules will be due to the lack of funds. To phase out chlorinated plastic bags, gloves, blood bags and to establish a bar code system for bags/containers the cost will be high and time span for doing this i.e. two years is too short.
Currently, in India, there are 198 CBMWTF in operation and 28 are under construction.[13] There is a great need for rapid development of many more CBMWTF to fulfill the need of treatment and disposal of all BMW generated in India. Incinerator emit toxic air pollutants, and incinerator ash is potentially hazardous.
Incinerator and its Hazards
The first solution for the disposal of BMW was to burn the waste. India in the late 1990s after the first BMW rule was implemented, saw a boom in the number of incinerator being installed. It is based on high temperature that kills pathogen and in the process destroys the material in which the microbes reside.[1415] However, a number of toxins are produced during its operation such as products of incomplete combustion (PIC) and dioxins. During incineration and postcombustion cooling, waste components dissociate and recombine forming new particles called PIC, which are toxic. Metals are not destroyed but are dispersed into the environment and these cause serious health issues. Dioxins are an unintentional by-product of waste combustion produced during incinerator operation. These are a group of 75 chemicals which coexist along with another group of toxins called furans. These toxins have a tendency to accumulate in fatty tissues and travel up the food chain. Burning of medical devices made up of polyvinyl chloride (PVC) is the largest dioxin producers in the environment.[16] In addition, metals present in the medical waste act as a catalyst for dioxin formation. These are very toxic, being known carcinogenic, and cause damage with immune and endocrine system of human. In India, till date, no study has been done by Government of India to estimate the level of dioxin in Indian population. In 2000, Subramanian et al. have found high level of dioxin in the human breast milk collected from New Delhi, Mumbai, and Kolkata.[17] Recently, in January 2017 appreciating the importance of the presence of dioxins in the environment, a joint project by Council of Scientific and Industrial Research and National Institute for Interdisciplinary Science and technology has started a study to analyze the presence of dioxins in Thiruvananthapuram.[18] Moreover, the incinerator ash is also hazardous and needs to be checked for the level of toxin before being sent to secured landfill. Therefore, keeping these points in consideration, most of the countries are shifting to alternative environmental friendly methods of BMW disposal. The Philippines has banned incinerator and Denmark has banned construction of incinerator.[1920]
Alternative Technology for Biomedical Waste Disposal
The various new technologies for BMW disposal are categorized into four groups – thermal, chemical processes, irradiative processes, and biological processes. Most of these are still under research.[21]
Thermal processes are grouped into three – low, medium, and high.
-
Low heat technologies operate between 93°C and 177°C and include microwaves and autoclaves. In autoclave, steam is used as a method for sterilization. Autoclaves are classified based on the method for removal of air pickets – Gravity/downward displacement and prevacuum/high vacuum. Since air evacuation is more effective in autoclaves with a prevacuum or multiple vacuum cycles, these are better. A shredder or grinder should be used if waste is to be made unrecognizable or reduction in waste volume is needed. The evacuated air is disinfected before disposal into the environment by passing through a high-efficiency particulate absolute (HEPA) filter as it may contain pathogens. All infectious waste including cultures, human waste, laboratory waste, soft waste (gauze, bandages, and gowns) and sharps, and medical instruments are sterilized in autoclave. Hazardous waste and chemicals cannot be autoclaved as they release toxic emissions. Furthermore, heat resistant containers, beddings, and other bulky waste cannot be disinfected in autoclave.[21] Microwave uses moist heat and steam generated by microwave energy to disinfect. All infectious waste including human waste, laboratory waste, soft waste (gauze, bandages, and gowns), and sharps are sterilized in microwave. Volatile, semi-volatile organic compounds, mercury, and radiological waste should not be put in microwave. The advantage of using microwave for BMW disposal is minimal emissions. Its disadvantage include requirement of high capital for setup, problem of odor near the machine, and there is a chance of leak of microwave energy
-
Medium heat technologies operate between 177°C and 540°C and include reverse polymerization and thermal depolymerization. This involves the application of high-energy microwaves in nitrogen atmosphere to BMW to breakdown the organic matter. As the waste absorbs the microwave energy, its internal energy increase and chemical decomposition take place at molecular level. Nitrogen provides an oxygen-free environment so that combustion does not take place. Then, shredders are used to mutilate the waste[21]
-
High heat technologies operate between 540°C and 8300°C and include pyrolysis – oxidation, plasma pyrolysis, induction-based pyrolysis, and lase-based pyrolysis. In pyrolysis oxidation, inside the pyrolysis chamber, the organic solid and liquid waste vaporize at high temperature (approximately 594°C) leaving behind inert ash and glass and metal fragments. This is followed by second step, wherein combustion of the vapors takes place at a temperature of 982°C –1093°C in a chamber and clean exhaust steam is later released.
Plasma pyrolysis uses plasma torches to generate plasma energy. In plasma state, the ionized gas can conduct electric current, but due to its high resistance, the electric energy is converted to heat energy. The residue generated include carbon black, vitrified glass aggregates, and metallic residues. A wide variety of waste can be destroyed in plasma-based technology – infectious waste, sharps, plastics, dialysis waste, hazardous waste, chemotherapeutic waste, chemotherapy waste, and low-level radioactive waste (one exemption is mercury which plasma systems do not handle). Many advantages of this system are low emission rate, waste residue is inert and sterile, i.e., environment friendly, and there is reduction in volume (95%) and mass (80%–90%). Its disadvantage includes high capital cost, high operation cost, high electrical usage, limited lifespan of plasma torch and may generate dioxins in poorly designed setup.[22]
Chemical-based technology
Many chemical used for BMW disposal are currently under development. The type of waste treated by chemical-based technology includes cultures, sharps, liquid waste, human waste, laboratory waste, and soft waste (gauze, bandages, and gowns). Volatile, semi-volatile organic compounds, mercury, and radiological waste should not be treated with chemical-based methods. The chemical-based technology requires closed system or is operated under negative pressure and the exhausted air has to be passed through HEPA to safeguard against aerosol formation during shredding. In chemical-based technology, shredding of BMW is must. The advantages of chemical-based technology include fully automated technique, easy to use, ease of discharge of liquid effluent into the sewage, and no by-products of combustion formed. The disadvantages include toxic by-products due to large-scale chlorine and hypochlorite use, chemical hazards, and often production of offensive odor. The chemical-based technology can be divided into chlorine- and nonchlorine-based systems.
The chlorine-based system uses sodium hypochlorite or chlorine dioxide. Sodium hypochlorite was one of the first chemical disinfectants used to treat BMW. Lately, it has been shown that toxins such as dioxins, halo acetic acid, and chlorinated aromatic compounds are released where sodium hypochlorite is used. Chlorine dioxide is unstable, so it is generated and used on-site. It is a strong biocide. It decomposes to form salt, less toxins are produced with its use, and it does not react with ammonium or alcohol.
Nonchlorine-based technologies use either gas, liquid, or dry chemical to treat BMW. Many of such system have come in market and few are discussed here. The SteriEcocycle 104 uses a portable chamber for collecting waste into which a peracetic acid-based decontaminant vial is added. After 10–12 min, peracetic acid disinfects the waste and aerosolized pathogens are prevented from escaping by use of HEPA filter. The liquid effluent is discharged into sewer and the waste goes as regular rash.[21]
Waste reduction (WR)[2] technology uses alkaline hydrolysis at high temperature to convert human and microbial waste into neutral aqueous solution. It is used for human/tissue waste, body fluids, and degradable bags. In addition, it can handle chemotherapy waste. The alkali also destroys fixative sin tissues and various hazardous chemicals such as glutaraldehyde and formaldehyde. This automated system has a steam-jacketed stainless steel container with a retainer for biodegradable waste such as bone and teeth.[21]
Lynntech's another technology uses ozone for decontamination of BMW. Being a strong oxidant, ozone destroys microbes and converts into molecular oxygen.[21]
Ionizing radiation cause damage to DNA and by producing free radicals cause further damage proteins and enzymes of infectious particles. The electron beam technology produces ionizing radiation in the form of a beam of high-energy electron propelled at high speed to strike the target. The waste to be treated are infectious waste including human waste, laboratory waste, soft waste (gauze, bandages, and gowns), and sharps. Volatile, semi-volatile organic compounds, mercury, and radiological waste should not be treated in electron beam units. The various advantages of this method are that it does not produce toxic emission, no liquid effluent, no ionizing radiation after machine is switched off, fully automated, and low operational cost. The disadvantage include protection from radiation exposure, concrete shield several feet thick around the system, removal of ozone gas, and there is no decrease in waste volume and need shredders or grinders.[21]
Biological methods for disposal of BMW include an emerging system called “Bio-converter” 9 Biomedical Disposal, Inc.). It uses a solution of enzyme to decontaminate medical waste, and the resulting sludge is put through an extruder used to remove water for sewage disposal and the solid waste is sent to landfill. Another method of environmental BMW disposal is the use of biodegradable plastics. Many biomedical implants built with biodegradable plastics undergo biological degradation with microbial extracellular enzymes. These microbes utilize these biodegradable polymers as substrate under starvation and in unavailability of suitable substrate. Further research needs to be done for large-scale economic manufacture of biodegradable plastics.[2123]
Conclusions
BMWM should be a shared teamwork with committed government backing, good BMW practices followed by both health-care workers and HCFs, continuous monitoring of BMW practices, and strong legislature. It is our fundamental right to live in clean and safe environment. The pillar of BMWM is segregation of waste at source and WR. The current BMWM 2016 rules are an improvement over earlier rules in terms of improved segregation, transportation, and disposal methods, to decrease environmental pollution and ensure the safety of the staff, patients, and public. Moreover, more use of non-PVC medical devices and development of newer novel, eco-friendly systems for disposal of BMW should be encouraged. All participants in BMWM should pledge to guarantee a cleaner and greener environment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Safe Management of Wastes from Health-Care Activities. (2nd). Geneva, Switzerland: WHO Press; 2014. p. :1-146.
- [Google Scholar]
- Physical and chemical composition of hospital waste. Infect Control Hosp Epidemiol. 1993;14:145-50.
- [Google Scholar]
- Review of Health Impacts from Microbiological Hazards in Health-Care Wastes. Geneva: World Health Organization; 2004.
- Secretariat of the Basel Convention. In: Technical Guidelines on Environmentally Sound Management of Wastes Consisting of Elemental Mercury and Wastes Containing or Contaminated with Mercury 31 October, 2011. Geneva: Basel Convention and United Nations Environment Programme; 2011.
- [Google Scholar]
- Secretariat of the Stockholm Convention. In: Revised Draft Guidelines on Best Available Techniques and Provisional Guidance on Best Environmental Practices of the Stockholm Convention on Persistent Organic Pollutants. Geneva: Secretariat of the Stockholm Convention; 2006.
- [Google Scholar]
- Countries: List of signatories. In: In: Minamata Convention on Mercury. Geneva: United Nations Environment Programme; 2014.
- [Google Scholar]
- Ministry of Environment and Forests Notification. In: Bio-Medical Waste (Management and Handling, 1998) Rules. New Delhi: Government of India Publications; 1998. p. :276-84.
- [Google Scholar]
- Bio-medical waste management: Situational analysis & predictors of performances in 25 districts across 20 Indian states. Indian J Med Res. 2014;139:141-53.
- [Google Scholar]
- Hepatitis B outbreak in Gujarat: A wake-up call. Indian J Med Ethics. 2009;6:120-1.
- [Google Scholar]
- The Gazette of India Biomedical Wastes (Management and Handling) Rules. India: Ministry of Environment and Forests, Government of India; Notification Dated; 20th July, 1998
- Bio-Medical Waste Management Rules 2016 Published in the Gazette of India, Extraordinary, Part II, Section 3, Sub-Section (i), Government of India Ministry of Environment, Forest and Climate Change. Notification; New Delhi, the 28th March, 2016
- Health effects associated with the disposal of solid waste in landfills and incinerators in populations living in surrounding areas: A systematic review. Int J Public Health. 2013;58:725-35.
- [Google Scholar]
- Available from: http://www.bsem.org.uk/uploads/IncineratorReport_v3.pdf
- Two decades of environmental surveillance in the vicinity of a waste incinerator: Human health risks associated with metals and PCDD/Fs. Arch Environ Contam Toxicol. 2015;69:241-53.
- [Google Scholar]
- High levels of organochlorines in mothers’ milk from Chennai (Madras) city, India. Chemosphere. 2007;68:928-39.
- [Google Scholar]
- Non-Incineration Medical Waste Treatment Technologies. Washington, DC: Health Care without Harm; 2001.
- [Google Scholar]
- Microbial enzymatic degradation of biodegradable plastics. Curr Pharm Biotechnol. 2017;18:429-40.
- [Google Scholar]





