Translate this page into:
Comparative Analysis of Enzyme-Linked Immunosorbent Assay and Immunochromatography for Rotavirus and Adenovirus Detection in Children below Five Years with Acute Gastroenteritis
Address for correspondence: Laxmi Kakhandaki, MBBS, MD, Department of Microbiology, BLDE(DU)'s Shri B. M. Patil Medical College, Hospital & Research Centre, Vijayapura, 586103, Karnataka, India (e-mail: laxmi.kakhandki@bldedu.ac.in).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction
The most frequent etiologies of viral gastroenteritis among young children are rotavirus and enteric adenovirus. The clinical signs and symptoms of viral gastroenteritis are not distinct enough to allow for diagnosis. For the diagnosis and treatment of acute gastroenteritis, it is preferable to use quick, simple, and low-cost procedures. This study was undertaken to determine efficacy of immune-chromatography test (ICT) in comparison with enzyme-linked immunosorbent assay (ELISA) to detect rotavirus and adenovirus antigen in fecal specimen among children less than 5 years of age with acute gastroenteritis.
Materials and Methods
In a cross-sectional observational study, 314 fecal samples were collected from children aged less than 5 years with acute gastroenteritis attending or admitted to a tertiary care hospital during the 1 year study period. Samples were tested for rotavirus and adenovirus antigen using ICT and ELISA.
Results
Among the 314 children evaluated, 112 (35.66%) had rotavirus infection, nine (2.86%) had adenovirus infection, and three (0.95%) had both rotavirus and adenovirus infection. This study found that ICT is 98.20% sensitive and 100% specific for the diagnosis of rotaviral diarrhea and 100% sensitive and 99.7% specific for adenovirus diarrhea, compared to ELISA.
Conclusion
Immunochromatography tests used for the detection of rotavirus and adenovirus in the fecal sample showed a high degree of sensitivity and specificity. The ICT is easy to perform and rapid, and it does not require any special equipment. Hence, the ICT could be used as an alternative method for detecting viral pathogens in clinical practice.
Keywords
diarrhea
rotavirus
adenovirus
ELISA
ICT
Introduction
Diarrheal disease that is both preventable and treatable and is the second leading cause of death in children under age of 5 globally.[1] Every year, approximately 1.7 billion cases of childhood diarrheal illness are reported, leading to the deaths of approximately 5,25,000 children under the age of 5, accounting for 8% of all deaths among them worldwide.[1,2] In India, diarrhea kills approximately 10% of children under the age of 5 accounting for 1.1 lakh deaths each year.[3]
Diarrhea is caused by various bacteria, parasites, or viruses, but in children less than 5 years, viruses are the main offenders.[4] Among the viruses, rotavirus is the leading cause of diarrhea in children under the age of 5 worldwide.[5] Rotavirus-related diarrhea is estimated to cause 2 million hospitalizations among children under the age of 5 each year, leading to approximately 199,000 young deaths worldwide.[6,7] Rotavirus is responsible for 34% of all diarrheal deaths in children under the age of 5 in India, with death rates higher in girls than boys.[8]
Human adenoviruses are also significant gastroenteritis pathogens, accounting for 1–20% of diarrheal disease cases among children under the age of 5 worldwide.[9,10]
Clinically, viral gastroenteritis is characterized by profuse diarrhea, mild fever, and vomiting, leading to mild-to-severe dehydration. The clinical manifestations of viral gastroenteritis alone are not sufficiently distinctive to permit diagnosis. Realizing that viral gastroenteritis causes severe diarrhea and is associated with high mortality especially in developing countries; there is need for timely diagnosis to initiate appropriate treatment and avoid unnecessary antibiotic usage.[7] Enzyme-linked immunosorbent assays (ELISA), latex agglutination, immunochromatography (ICT), and real-time polymerase chain reaction (RT-PCR) are some of the diagnostic possibilities for viral gastroenteritis.[11] It is desirable to use rapid, easy, and cost-effective methods for diagnosis and management of acute gastroenteritis. The enzyme immunoassay approach is sensitive, but it takes several hours to complete the test, whereas the ICT is simple, quick, and inexpensive. There have been few studies comparing ICT to ELISA for detecting rotavirus and adenovirus antigen in feces in patients with acute gastroenteritis.[12-15] Hence, this study was undertaken to determine the efficacy of ICT in comparison with ELISA to detect rotavirus and adenovirus antigen in fecal specimen among children less than 5 years of age with acute gastroenteritis.
Materials and Methods
This was a cross-sectional observational study, carried out in the department of microbiology, at our tertiary care hospital, South India. Single fecal sample was collected from each of the 314 children aged less than 5 years with acute gastroenteritis attending or admitted to hospital during the study period of January to December 2018. The study protocol was approved by the ethical committee of our institute. Sample was collected after obtaining informed consent from parents or guardians of the pediatric subjects. Demographic and relevant clinical data was collected from each child. The fecal samples were subjected to macroscopic examination for color, consistency, presence of mucus, and blood. The samples were also examined microscopically for presence of red blood cells, leucocytes, parasitic ova and cysts in saline and iodine preparations. Feces showing presence of blood or parasites were excluded from the study. The feces samples included in the study were then subjected to ELISA and ICT for rotavirus and adenovirus antigen detection. Feces samples were stored at −20°C until assayed for the detection of rotavirus and adenovirus antigen.
Enzyme-Linked Immunosorbent Assay
Detection of Rotavirus Antigen
A sandwich type ELISA (RIDASCREEN Rotavirus, r-Biophram GmbH Darmstadt, Germany) was used for the detection of rotavirus antigen in fecal sample. Suspension of diluted fecal samples (1:10) were added to microwells coated with monoclonal antibodies to VP6 gene product that is group-specific antigen of human rotaviruses together with biotinylated monoclonal antirotavirus antibodies (conjugate 1). After a wash step, monoclonal antirotavirus antibodies conjugated with polystreptavidin peroxidase (conjugate 2) were added. If rotaviruses are present in the fecal sample, a sandwich complex was formed made up of the immobilized antibodies, the rotavirus antigens, and the antibodies conjugated with the biotin streptavidin peroxidase complex. If the test was positive, after adding the substrate (hydrogen peroxide/3,3′,5,5′-tetramethylbenzidine [TMB]), the attached enzyme changed the color of the previously colorless solution in the microwells to blue. On adding the stop reagent (1 M sulfuric acid), the color changed from blue to yellow. Photometric measurement of microwells was carried out at 450 nm and results were interpreted according to manufacturer's instructions.[16]
Detection of Adenovirus Antigen
A sandwich-type ELISA (RIDASCREEN Adenovirus, r-Biophram GmbH Darmstadt, Germany) was used for the detection of adenovirus antigen in fecal sample. Suspension of diluted fecal samples (1:10) was added to microwells coated with monoclonal antibodies to hexon antigen of adenoviruses together with biotinylated monoclonal anti-Adenovirus antibodies (conjugate 1). After a wash step, monoclonal antiadenovirus antibodies conjugated with polystreptavidin peroxidase (conjugate 2) were added. If adenoviruses are present in the fecal sample, a sandwich complex was formed made up of the immobilized antibodies, the adenovirus antigens, and the antibodies conjugated with the biotin–streptavidin–peroxidase complex. If the test was positive, after adding the substrate (hydrogen peroxide/TMB), the attached enzyme changed the color of the previously colorless solution in the microwells to blue. On adding the stop reagent (1 M sulfuric acid), the color changed from blue to yellow. Photometric measurement of microwells was carried out at 450 nm and results were interpreted according to manufacturer's intructions.[17]
Immunochromatography Test
The ICT (RIDA QUIK, r-Biopharm, GmbH Darmstadt, Germany) was a single-step lateral-flow assay for the determination of both rotavirus and adenovirus antigen in fecal samples. The strip was immersed into the clear supernatant of diluted fecal sample (1:10) up to the arrow mark. The sample passed with the colored latex particles to which the antigens were attached if the test was positive, through the membrane and bound to the specific collection bands. The result was read after 5 minutes. The presence of blue and green bands indicated that the sample was positive for adenovirus, while the presence of red and green bands indicated that the sample was positive for rotavirus. The presence of blue, red, and green bands indicated that the sample was positive for both adenovirus and rotavirus, while the presence of only the green band indicated that the sample was negative for both rotavirus and adenovirus.[18]
Statistical Methods Used
Statistical analysis was performed by the SPSS program, version 20.0. Continuous variables are presented as mean ± standard deviation, and categorical variables are presented as absolute numbers and percentage. Statistical analysis considered sensitivity, specificity, positive-predictive value and negative-predictive value.
Results
A total of 314 nonrepetitive fecal samples from children less than 5 years of age with acute gastroenteritis were obtained during the study period. All the fecal samples were tested for rotavirus and adenovirus antigen. Out of the 314 children with acute gastroenteritis, 197 were males and 117 females with mean age of 15.94 ± 13.1 months.
In this study, infection with at least one viral agent was seen among 124 (39.49%) children that was detected by either ELISA or ICT test. Among the 124 children tested positive, 112 (35.66%) had rotavirus infection, 9 (2.86%) had adenovirus infection, and 3 (0.95%) had both rotavirus and adenovirus infection.
Among the 112 children with rotavirus gastroenteritis, 71 (63.39%) were male and 41(36.6%) female (►Table 1). The majority of rotavirus-positive cases (47.32%, 53/112) were in the age group of 7 to 12 months, with 91.96% (103/112) of rotavirus-positive cases being under the age of 24 months (►Table 2). Infection occurred throughout the year, with peak rotavirus infection occurring in the month of January (21.42%, 24/112) followed by December (19.64%, 22/112) and February (14.28%, 16/112) (►Fig. 1). Significant proportion of children infected with rotavirus presented with vomiting (81.25%), dehydration (67.85%), and watery diarrhea (60.7%). Fever was present in 56.25% of children with rotavirus diarrhea. Stool consistency in a significant proportion of children with rotavirus diarrhea was liquid/watery (45.53%) and semisolid (41.07%) (►Table 3).
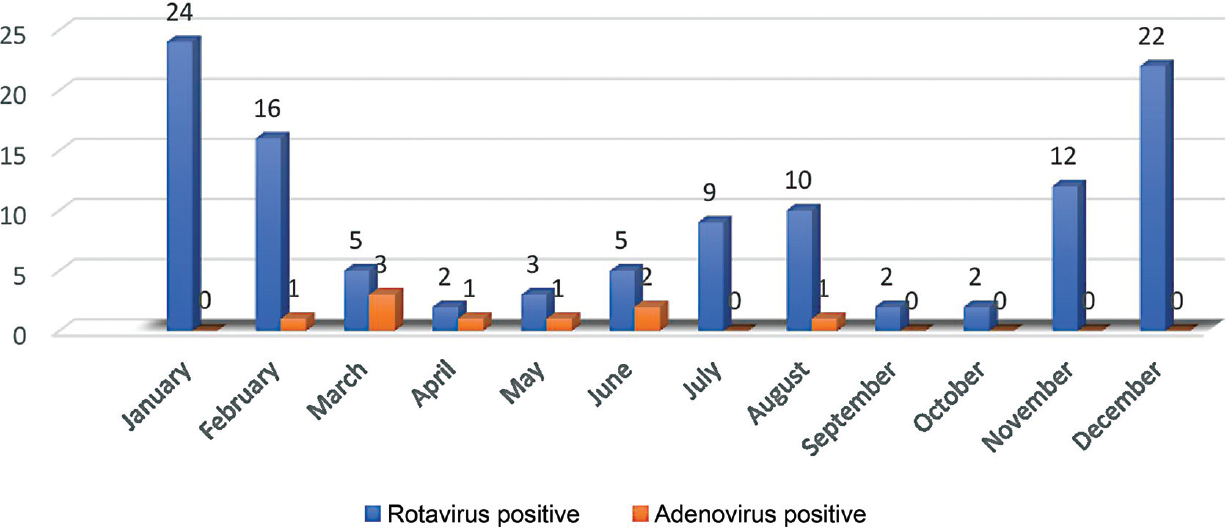
- Month-wise distribution of number of rotavirus and adenovirus-positive children with age less than 5 years.
| Sex | Total tested | Rotavirus positive, n (%) | Adenovirus positive, n (%) | Rotavirus and adenovirus positive, n (%) |
|---|---|---|---|---|
| Male | 197 | 71 (63.39) | 8 (88.88) | 2 (66.66) |
| Female | 117 | 41 (36.6) | 1 (11.11) | 1 (33.33) |
| Total | 314 | 112 | 9 | 3 |
| Age in months | Total tested | Rotavirus positive | Adenovirus positive | Rotavirus and adenovirus positive | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| ≤ 6 | 62 | 20 | 17.85 | 2 | 22.22 | 1 | 33.33 |
| 7–12 | 111 | 53 | 47.32 | 6 | 66.66 | 2 | 66.66 |
| 13–24 | 76 | 30 | 26.78 | 0 | 0 | 0 | 0 |
| 25–36 | 34 | 6 | 5.35 | 0 | 0 | 0 | 0 |
| 37–60 | 31 | 3 | 2.67 | 1 | 11.11 | 0 | 0 |
| Clinical parameter | Rotavirus positive (n = 112) | Adenovirus positive (n = 9) | ||
|---|---|---|---|---|
| n | % | n | % | |
| Vomiting | 91 | 81.25 | 2 | 22.22 |
| Dehydration | 76 | 67.85 | 3 | 33.33 |
| Watery diarrhea | 68 | 60.7 | 5 | 55.55 |
| Fever | 63 | 56.25 | 0 | 0 |
| Abdominal pain | 37 | 33.03 | 3 | 33.33 |
| Feces consistency | ||||
| Liquid/watery | 68 | 60.7 | 5 | 55.55 |
| Semisolid | 29 | 25.89 | 4 | 44.44 |
| Unformed | 15 | 13.39 | 0 | 0 |
Among nine adenovirus-positive children, eight were male and one was female (►Table 1). Major proportion (66.66%, 6/9) of the adenovirus-positive cases was in the age group of 7 to 12 months with 88.88% (8/9) of adenovirus-positive cases belonging to age 12 months or younger (►Table 2). Peak adenovirus infection occurred in the month of March (33.33%, 3/9) followed by June (22.22%, 2/9) (►Fig. 1). Significant proportion of children infected with adenovirus presented with watery diarrhea (55.55%), dehydration (33.33%), and vomiting (22.22%). Feces was watery in a major proportion (55.55%) of the children infected with adenovirus (►Table 3).
In three children with acute gastroenteritis, both rotavirus and adenovirus antigens were detected. Among these three children, two were male and one female. One of the patients was less than 6 months of age, while two belonged to the age group of 7 to 12 months. One case occurred each in the months of May, June, and August. Dehydration was seen in all the patients, while fever and vomiting were present in two of the patients. Consistency of feces was liquid in two cases and semisolid in one case (not represented in table)
Rotavirus antigen was detected in 112 samples by ELISA, while in 110 samples by ICT (►Table 4). Considering ELISA as the gold standard, the sensitivity, specificity, positive predictive value, and negative predictive value of ICT test were 98.2, 100, 100, 99%, respectively. Adenovirus antigen was detected in nine samples by ICT, while eight specimens were positive by ELISA (►Table 5). Considering ELISA as the gold standard, the sensitivity, specificity, positive predictive value, and negative predictive value of ICT test were 100, 99.7, 99.4, 100%, respectively.
| Immunochromatography test | Enzyme-linked immunosorbent assay | |
|---|---|---|
| Positive | Negative | |
| Positive | 110 | 0 |
| Negative | 2 | 202 |
| Immunochromatography test | Enzyme-linked immunosorbent assay | |
|---|---|---|
| Positive | Negative | |
| Positive | 8 | 1 |
| Negative | 0 | 305 |
Discussion
Acute gastroenteritis is a common disease seen in all ages and continues to be one of the most common causes of death among all ages.[4,19] Young children and elderly people have predilection for dehydration leading to severe complications.[19] Acute gastroenteritis that is characterized by inflammation of gastrointestinal tract is caused by viruses, bacteria, or parasites.[5,20] Among them enteric viruses are the most significant etiological agents of acute gastroenteritis, accounting to 70% of diarrheal episodes in young children.[20] Rotavirus is the leading cause of diarrhea in children under the age of 5 worldwide, with high rates of morbidity and fatality.[4] Among the 10 species, termed as rotavirus A to rotavirus J, rotavirus A is clinically the most significant species worldwide.[19] Each year, rotavirus affects an estimated 11.37 million episodes of acute gastroenteritis in children under the age of 5 in India, necessitating 3.27 million outpatient visits and 872,000 hospitalizations, totaling INR 10.37 billion in direct expenses.[21] Rotavirus is estimated to be responsible for 40% of all acute gastroenteritis-related hospitalizations in children under the age of 5.[22] Enteric adenoviruses have also been found to be a common cause of viral gastroenteritis in children. Adenovirus serotypes 40 and 41 are responsible for 1 to 20% of diarrheal illness cases in both outpatients and hospitalized children worldwide.[23] Adenoviral diarrhea is characterized by watery, nonbloody diarrhea that lasts 2 to 22 days and is accompanied by mild fever and vomiting.[24] Several times, it is not easy to distinguish viral gastroenteritis from gastroenteritis caused by bacterial agents clinically, and laboratory tests are required to make a definite diagnosis.[19]
Rotavirus was responsible for a significant proportion (35.66%) of acute gastroenteritis in children less than 5 years in this study. This finding is comparable with reports obtained by EI Qazoui et al[25] (26.6%) and Shetty et al[26] (28.57%). Adenoviruses accounted for 2.86% of acute gastroenteritis cases in our study. Incidence of human adenoviruses causing childhood gastroenteritis is reported to be 5.18% by Sanaei Dashti et al,[27] 31.2% by Ouédraogo et al,[28] 7.2% by Kumthip et al.[29]
In this study, high prevalence of rotavirus gastroenteritis was seen among males (63.39%) that is in agreement with results of previous studies where 65.71%[26] and 53.9%[25] pediatric patients were male. Male dominance (88.88%) was also seen among adenovirus gastroenteritis cases that is similar to findings seen in other studies, that is 62.87[27] and 54%.[29] The male prevalence can be explained by a societal reason: parents' predisposition to prefer their male children above their female offspring when seeking health care. This can potentially be explained by females having a higher resistance to infection due to the XX chromosome.[12]
In our study, the majority of rotavirus-infected children were under the age of 2 years, with the highest frequency occurring between the age group of 7 to 12 months (47.32%). This age distribution is comparable with reports obtained by EI Qazoui et al[25] (36%). Adenovirus-infected children with gastroenteritis were also seen among under 2 years of age with the majority of the cases in the 7 to 12 months age group (66.66%) that are in accordance with findings of Sanaei Dashti et al[27] (58.3%). In the children aged between 0 and 6 months, low incidence rate may be due to passive immunity attained by the infants from their mothers, which tapers after 6 months, or even the higher rate of breast feeding in this age group, which also protects the infants via the transmission of immunoglobulin A antibodies. By the age of 3, all humans will have at least one episode of rotavirus infection, with rotavirus antibodies remaining in circulation indefinitely, providing protection against rotavirus infection and disease, resulting in a lower rate of rotavirus gastroenteritis in older children.[30]
Rotavirus infections were predominantly seen during winter months, that is, December to February. Similar findings were reported by Muhsen et al,[31] Gupta et al,[32] Giri et al,[33] and EI Qazoui et al.[25] In this study, highest adenovirus infections were seen during the month of March (33.33%) followed by June (22.22%). Kumthip et al[29] and Banerjee et al[34] observed highest rates of adenovirus infection in the period of May to July.
Symptoms like vomiting (81.25%) and dehydration (67.85%) were predominantly seen in rotavirus gastroenteritis cases. Watery feces (60.7%) were frequently seen in rotavirus-positive cases. The similar findings were observed in the study conducted by Mukaratirwa et al.[35] In a study conducted by EI Qazoui et al,[25] vomiting episodes of 5 or more per day was identified in 73.08% of children infected with rotavirus, while 20.51% experienced two to four vomiting episodes per day. Severe dehydration was found in 56.41% of children, whereas moderate dehydration was found in 33.33%.[25]
This study found that ICT is 98.20% sensitive and 100% specific for diagnosis of rotaviral diarrhea compared to ELISA. This finding is in agreement with Dhiman et al[12] and Salwa et al.[13] Considering ELISA as gold standard, Dhiman et al[12] compared ICT with ELISA and found the sensitivity and specificity of ICT to be 95.24 and 97.47%, respectively and Salwa et al[13] found sensitivity and specificity of ICT 90.0 and 100%, respectively. These findings suggest that results of ICT and ELISA are fairly comparable and hence ICT can be used in clinical practice for rapid detection of rotavirus infection. Kim J. et al[15] compared ICT with ELISA, ELFA (enzyme linked fluorescent assay), RT-PCR, and multiplex reverse transcription PCR and found that overall agreement among the four methods for rotavirus detection was 91.5% and adenovirus detection was 85.5%. Therefore, they concluded that the ICT method can be useful in clinical practice for the rapid detection of rotavirus and adenovirus infection. González-Serrano et al[36] compared ICT to PCR for rotavirus and adenovirus detection in patients with acute gastroenteritis, and the results showed high specificity (> 97%) and sensitivity (> 80%).
Conclusion
An accurate diagnosis of viral gastroenteritis is essential since it obviates the unnecessary use of antibiotic therapy. The rapid diagnosis of viral gastroenteritis in patients with symptoms of gastroenteritis would enable better treatment of the patients. In this study, we evaluated ICT for the detection of rotavirus and adenovirus in the fecal sample. It showed a high degree of sensitivity and specificity. The ICT is simple to perform, provides a quick diagnosis, and does not require any special equipment. As a result, the ICT could be used in clinical practice as an alternative method for detecting viral pathogens in fecal samples.
Authors' Contributions
S.B. contributed to conceptualization, design, definition of intellectual content, literature search, data acquisition, data analysis, manuscript preparation, and manuscript editing. L.K. was involved in literature search, data acquisition, data analysis, manuscript preparation, and manuscript editing. R.K. was involved in literature search, data acquisition, and manuscript editing. S.W. analyzed the data and edited the manuscript. P.S. edited and reviewed the manuscript. M.M.P. was involved in data acquisition, manuscript editing and review.
Conflict of Interest
None declared.
References
- Who.int. Published 2021. Accessed June 13, 2022 https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease
- [Google Scholar]
- UNICEF DATA. Published 2021. Accessed June 13, 2022 https://data.unicef.org/topic/child-health/diarrhoeal-disease/
- [Google Scholar]
- Diarrheal diseases among children in India: current scenario and future perspectives. J Nat Sci Biol Med. 2015;6(01):24-28.
- [CrossRef] [PubMed] [Google Scholar]
- Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis. 2018;18(11):1211-1228.
- [Google Scholar]
- GBD Diarrhoeal Diseases Collaborators. Estimates of global, regional, and national morbidity, mortality, and aetiologies of diarrhoeal diseases: a systematic analysis for the Global Burden of Disease Study 2015. published correction appears in Lancet Infect Dis. 2017;17(9):897. Lancet Infect Dis 2017; 17 (09) 909-948
- [Google Scholar]
- Epidemiology of rotavirus gastroenteritis and need of high rotavirus vaccine coverage with early completion of vaccination schedule for protection against rotavirus diarrhea in India: A narrative review. Indian J Public Health. 2019;63(03):243-250.
- [CrossRef] [PubMed] [Google Scholar]
- Global illness and deaths caused by rotavirus disease in children. Emerg Infect Dis. 2003;9(05):565-572.
- [CrossRef] [PubMed] [Google Scholar]
- Million Death Study Collaborators. Rotavirus mortality in India: estimates based on a nationally representative survey of diarrhoeal deaths. Bull World Health Organ. 2012;90(10):720-727.
- [CrossRef] [PubMed] [Google Scholar]
- Diversity in the enteric viruses detected in outbreaks of gastroenteritis from Mumbai, Western India. Int J Environ Res Public Health. 2012;9(03):895-915.
- [CrossRef] [PubMed] [Google Scholar]
- Circulation of a novel pattern of infections by enteric adenovirus serotype 41 among children below 5 years of age in Kolkata, India. J Clin Microbiol. 2011;49(02):500-505.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of viral gastroenteritis: limits and potential of currently available procedures. J Infect Dev Ctries. 2015;9(06):551-561.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of enzyme-linked immunosorbent assay and immunochromatography for rotavirus detection in children below five years with acute gastroenteritis. J Clin Diagn Res. 2015;9(09):DC06-DC09.
- [CrossRef] [PubMed] [Google Scholar]
- A comparative study of rotaviral antigen detection by ELISA and ICT in children below five years with acute diarrhoea in a tertiary care hospital. Bangladesh Med J. 2021;49(01):14-18.
- [CrossRef] [Google Scholar]
- Evaluation of an immunochromatographic assay for the rapid and simultaneous detection of rotavirus and adenovirus in stool samples. Ann Lab Med. 2014;34(03):216-222.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Diagnostics. Published 2012. Accessed June 13, 2022 https://clinical.r-biopharm.com/products/ridascreen-rotavirus/
- [Google Scholar]
- Clinical Diagnostics. Published 2010. Accessed June 13, 2022 https://clinical.r-biopharm.com/products/ridascreen-adenovirus/
- [Google Scholar]
- Docplayer.net. Published 2014. Accessed June 13, 2022 https://docplayer.net/118402003-Rida-quick-rotavirus-adenovirus-combi.html
- [Google Scholar]
- Acute gastroenteritis: from guidelines to real life. Clin Exp Gastroenterol. 2010;3:97-112.
- [CrossRef] [PubMed] [Google Scholar]
- Rotavirus gastroenteritis in India, 2011-2013: revised estimates of disease burden and potential impact of vaccines. Vaccine. 2014;32(Suppl 1):A5-A9.
- [CrossRef] [PubMed] [Google Scholar]
- Indian Rotavirus Strain Surveillance Network. Diversity of circulating rotavirus strains in children hospitalized with diarrhea in India, 2005-2009. Vaccine. 2013;31(27):2879-2883.
- [CrossRef] [PubMed] [Google Scholar]
- Characterizations of adenovirus type 41 isolates from children with acute gastroenteritis in Japan, Vietnam, and Korea. J Clin Microbiol. 2004;42(09):4032-4039.
- [CrossRef] [PubMed] [Google Scholar]
- Importance of enteric adenoviruses 40 and 41 in acute gastroenteritis in infants and young children. J Clin Microbiol. 1984;20(03):365-372.
- [CrossRef] [PubMed] [Google Scholar]
- Rotavirus and norovirus infections among acute gastroenteritis children in Morocco. BMC Infect Dis. 2014;14(01):300.
- [CrossRef] [PubMed] [Google Scholar]
- Detection of rotavirus and adenovirus diarrhea in children below five years, in Dakshina Kannada District, a coastal region of Karnataka State, India. Muller J Med Sci Res. 2014;5:143-148.
- [CrossRef] [Google Scholar]
- Molecular epidemiology of enteric adenovirus gastroenteritis in under-five-year-old children in Iran. Gastroenterol Res Pract. 2016;2016 2045697
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and genetic diversity of enteric viruses in children with diarrhea in Ouagadougou, Burkina Faso. PLoS One. 2016;11(04):e0153652.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple enterovirus genotypes circulating in children hospitalized with acute gastroenteritis in Thailand. Infect Genet Evol. 2017;55:324-331.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of rotavirus infection in children with gastroenteritis attending Jos university teaching hospital, Nigeria. Virol J. 2011;8:233.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and characteristics of sporadic norovirus gastroenteritis associated with hospitalization of children less than 5 years of age in Israel. Pediatr Infect Dis J. 2013;32(06):688-690.
- [CrossRef] [PubMed] [Google Scholar]
- Aetiology of childhood viral gastroenteritis in Lucknow, North India. Indian J Med Res. 2015;141(04):469-472.
- [CrossRef] [PubMed] [Google Scholar]
- Rotavirus gastroenteritis in Indian children < 5 years hospitalized for diarrhoea, 2012 to 2016. BMC Public Health. 2019;19(01):69.
- [CrossRef] [PubMed] [Google Scholar]
- Molecular characterization of enteric adenovirus genotypes 40 and 41 identified in children with acute gastroenteritis in Kolkata, India during 2013-2014. J Med Virol. 2017;89(04):606-614.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiologic and genotypic characteristics of rotavirus strains detected in children less than 5 years of age with gastroenteritis treated at 3 pediatric hospitals in Zimbabwe during 2008-2011. Pediatr Infect Dis J. 2014;33(Suppl 1):S45-S48.
- [CrossRef] [PubMed] [Google Scholar]
- Viral gastroenteritis in hospitalized patients: evaluation of immunochromatographic methods for rapid detection in stool samples. J Clin Virol. 2020;128 104420
- [Google Scholar]






