Translate this page into:
Contiguous Lumbar Vertebral Involvement with Vertebral Collapse in Giant Cell Tumor: A Usual Tumor with an Unusual Presentation
Address for correspondence: Ruchita Tyagi, MD, DNB, Department of Pathology, Dayanand Medical College and Hospital, Tagore Nagar, Ludhiana, Punjab 141101, India (e-mail: ruchitatyagi@gmail.com).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Giant cell tumor (GCT) is a primary bone tumor of long bones, which can rarely involve the vertebrae. Contiguous vertebral involvement by GCT is a rare presentation and poses a diagnostic dilemma on imaging. We report a case of GCT involving three contiguous lumbar vertebrae causing vertebral collapse along with a large soft tissue component. Considering the site and clinical presentation, possibilities of a round cell tumor with large extraosseous soft tissue component and malignant neurogenic tumor were suggested on initial radiological examination but histopathology confirmed the diagnosis of GCT. It is important to diagnose this entity correctly because of totally different lines of management. In our case, initial surgical management was excluded in view of high surgical morbidity and, thereby, adjuvant therapy with denosumab was planned.
Keywords
lumbar
vertebrae
giant cell tumor
Introduction
Giant cell tumor (GCT) is a rare primary bone tumor of adults, involving the epiphysis of long bones. The most common sites are distal femur, distal radius and sacrum. In spine, this tumor occurs in sacrum followed by thoracic, cervical and lumbar vertebra in the decreasing order of frequency. Vertebral column involvement by GCT is very rare and contiguous involvement of lumbar vertebrae is rarer still.[1] This clinical scenario was mistaken to be round cell tumor on imaging, and the final diagnosis was rendered on histopathology.
Clinical Details
A 28-year-old female patient presented with progressive weakness of bilateral lower limbs for last 3 months. She had urinary and bowel incontinence, for which she had been catheterized 2 days prior to admission. There was significant weight loss of 7 kg and dull aching pain in the lower back for last 6 months. There was no history of fever, cough, recent trauma, or any prior illnesses such as tuberculosis, diabetes, or any other chronic ailments.
General physical examination revealed pulse rate 76 beats per minute, blood pressure 132/82 mm of mercury, and respiratory rate 16 per minute. A diffuse, mildly tender, and non-pulsatile swelling was noted in the lower lumbar region. Neurological examination revealed bilateral absence of lower limb deep tendon reflexes, bilateral lower limb weakness (three out of five), decreased sensation of temperature, pain, and proprioception. Erythrocyte sedimentation rate was 72 mm in the first hour (normal range 0–20 mm) and hemoglobin was 9.8 g/dL (normal range 12–15 g/dL). Other laboratory parameters including corrected serum calcium, serum alkaline phosphatase, and serum albumin levels were within normal limits. Baseline radiological investigations such as chest roentgenogram and non-contrast computerized tomography of the brain were normal. Radiographic appearance and NCCT scan of lumbar region showed complete collapse of L3 vertebra with extension of lytic destruction into both the pedicles of L3 vertebra. Large areas of lytic destruction were also seen in the L4 vertebral body. No significant septations within the lesion or sclerosis was seen around margins of lytic area. The intervertebral discs were not involved by the disease process.
Magnetic resonance imaging (MRI) (►Fig. 1) of her spine showed T2 iso- to hypointense signal intensity soft tissue involving L2, L3, L4 vertebral bodies with collapse of the L3 vertebra. The soft tissue showed heterogenous enhancement on post gadolinium images. It was also infiltrating into the right L2-L3 and L3-L4 neural foramina with extension into anterior epidural space compressing the spinal canal and cauda-equina nerve roots. The intervertebral discs were spared. The soft tissue appeared isointense to paraspinal muscles on T1-weighted images. Additionally, scattered T1 and T2 hypointense areas were seen within it. Multiple large T2 hyperintense cystic areas were seen in the extraosseous soft tissue. On initial radiological evaluation, possibilities of round cell tumor with large extraosseous soft tissue component and malignant neurogenic tumor were considered. Histopathological examination of trucut biopsy (►Fig. 2) showed a giant cell lesion comprising of mononuclear cells with interspersed, uniformly distributed, numerous multinucleated giant cells. The nuclei of these giant cells were similar to those of mononuclear cells. No blood-filled spaces, nuclear pleomorphism, or significant mitotic activity was identified. Therefore, a histopathological diagnosis of giant cell tumor of lumbar vertebra with soft tissue component was rendered, which came as a surprise to the radiologist. Radiological features were revised with extensive literature search and after correlating with histopathology, a final radiological diagnosis of this being GCT with contiguous lumbar vertebral involvement (L2-L4) causing vertebral collapse along with a large soft tissue component was proposed and an excisional biopsy was advised. Due to its location and extent, the tumor was inoperable. The treatment plan included adjuvant therapy with subcutaneous denosumab therapy, followed by surgery.
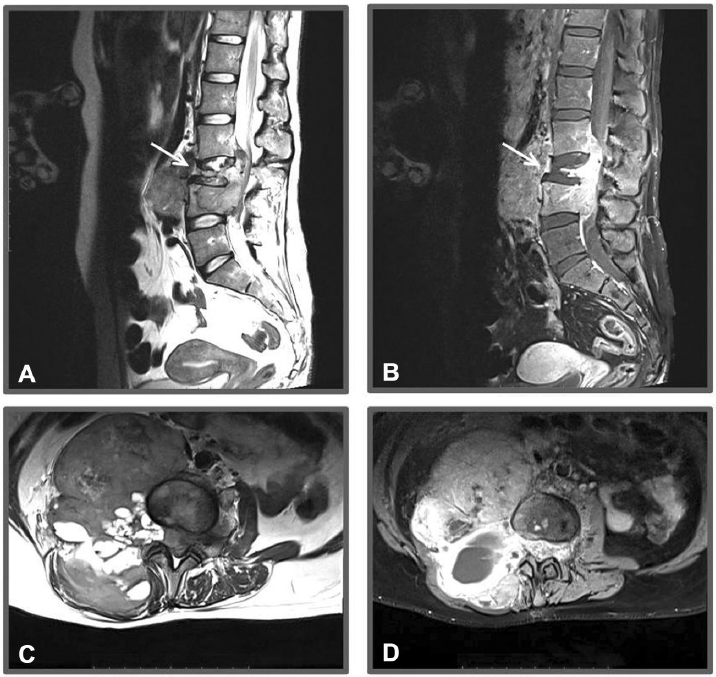
- MRI. (A and B) (T2-weighted and post-contrast sagittal images respectively) and (C and D) (T2-weighted and post-contrast axial images respectively) showing the collapse of L3 vertebra (white arrow) with contiguous involvement of L2 and L4 vertebra with large soft tissue component on the right side.

- Hematoxylin and eosin-stained sections of mass showing (A) giant cell lesion composed of mononuclear cells with interspersed, uniformly distributed numerous multinucleated giant cells. (100×) (B) Nuclei of giant cells are similar to those of stromal cells (400×).
Discussion
Giant cell tumor accounts for 5% of primary bone tumors and spinal involvement occurs only in around 1.5% of these cases.[1] There is equal gender predilection and age group affected is 20–45 years.[2,3] Our patient was 28 years old, which corroborates with the age of GCT. GCT involving vertebrae is an uncommon occurrence and only a few such cases have been reported.[2-5] In this case, contiguous involvement of adjacent vertebrae is an unusual finding, which posed a diagnostic challenge on radiology. Contiguous involvement of vertebra more commonly occurs in infections such as tuberculosis.[6] The patient did not complain of any fever, thus eliminating the likelihood of an infectious etiology. On radiology, there was no para-discal involvement or cystic area in soft tissue. Considering the site and clinical presentation, initial radiological possibilities included round cell tumor with large extraosseous soft tissue component and malignant neurogenic tumor. The imaging in axial lesions may not confirm the diagnosis but it can guide the most representative site that should be biopsied. The usual radiological features of spinal GCT include expansile lesion with lytic characteristic. The spinal GCT is usually not associated with mineralized matrix. The vertebral lesions are usually large and involve adjacent soft tissues. MRI reveals iso- to hypointense signal intensity on T1 and heterogeneous high intensity on T2-weighted images. The intramedullary tumor is best seen on T1W, whereas extraosseous soft tissue component is best appreciated on T2W image due to the presence of increased collagen content. This feature helps to differentiate GCT from other spinal neoplasms such as metastases, lymphomas, and chordoma that usually demonstrate hyperintense signal on T2-weighted MR images.[2-4,6,7] The symptoms are caused by nerve root compression leading to radiculopathy and sensory and motor deficit of variable severity, as in our case. It is a locally aggressive tumor, as also described in this case.[2,3,8]
The importance of correct diagnosis lies in directed management. The treatment of GCT is complete surgical excision, as the tumor rarely metastases. However, when GCT involves the vertebrae, complete surgical resection may not be possible because of its locally aggressive nature. In such scenarios, treatment options include local radiation therapy, chemo-embolization, or systemic therapies such as bisphosphonates, sunitinib, calcitonin, or denosumab.[2,3,5,9,10] In this case, the patient was started on adjuvant therapy with denosumab. Subsequently, she will be followed for clinical improvement and tumor size regression, based on which a decision for the extent of surgery will be taken.
The rarity of a GCT causing lumbar vertebral collapse prevented the radiologist from considering it as the first possibility. The diagnosis could only be confirmed on histopathology, which prompted the radiologist to revise the radiological diagnosis and helped in the targeted management of the tumor.
Authors' Contributions
A.S., D.S.D., and R.T. contributed to concept and design of the study, definition of intellectual content, literature search, clinical studies, experimental studies, data acquisition and analysis. A.S. and D.S.D. contributed to statistical analysis and manuscript editing. A.K.C. contributed to definition of intellectual content, literature search, clinical studies, experimental studies, and data acquisition and analysis. H.K. contributed to definition of intellectual content, clinical studies, data acquisition and analysis, statistical analysis and manuscript editing and reviewing. N.S. contributed to the study concept, definition of intellectual content, clinical and experimental studies, data analysis, and manuscript editing and reviewing. H.K. and N.S. are the guarantors of the study.
Conflict of Interest
None declared.
Funding
None.
References
- Giant cell tumor of dorsal vertebral body. J Craniovertebr Junction Spine. 2012;3(02):67-69.
- [CrossRef] [PubMed] [Google Scholar]
- Giant cell tumor of dorsal vertebrae-a rare case report with review of literature. Adv Cytol Pathol. 2017;2:68-70.
- [CrossRef] [Google Scholar]
- Giant cell tumor of the spine: a review of 9 surgical interventions in 6 cases. Indian J Orthop. 2007;41(02):146-150.
- [CrossRef] [PubMed] [Google Scholar]
- Recurrent giant cell tumour of the thoracic spine managed by total en bloc spondylectomy and denosumab therapy: a case report. BMC Musculoskelet Disord. 2020;21(01):105.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging assessment of the spine: infection or an imitation? Radiographics. 2009;29(02):599-612.
- [CrossRef] [PubMed] [Google Scholar]
- Infections of the spinal column–spondylodiscitis. Diagn Interv Imaging. 2012;93(06):520-529.
- [CrossRef] [PubMed] [Google Scholar]
- Giant cell tumor of the sacrum. Neurosurg Focus. 2003;15(02):E13.
- [CrossRef] [PubMed] [Google Scholar]
- Denosumab in patients with giant-cell tumour of bone: an open-label, phase 2 study. Lancet Oncol. 2010;11(03):275-280.
- [CrossRef] [PubMed] [Google Scholar]
- Bisphosphonate treatment of aggressive primary, recurrent and metastatic giant cell tumour of bone. BMC Cancer. 2010;10:462.
- [CrossRef] [PubMed] [Google Scholar]





