Translate this page into:
Occurrence of Needlestick and Injuries among Health-care Workers of a Tertiary Care Teaching Hospital in North India
Address for correspondence: Prof. Sarman Singh, E-mail: sarman_singh@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Occupational hazards such as accidental exposure to sharp, cuts, and splashes are common among health-care workers (HCWs).
Aims and Objectives:
To determine the occurrence of self-reported occupational exposures to these hazards and to know the prevalent practices following the exposure. The second aim was to know the baseline antibody levels against hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV) immediately after these accidents.
Methods:
An observational prospective study was done in the HCWs of a tertiary care academic health organization of North India from January 2011 to December 2013. At the time of self-reporting of injury, a questionnaire was administered. Blood sample of HCWs and of the source, if identified, was collected for baseline HBV, HCV, and HIV serum markers. The exposed HCWs were followed up and repeat testing was done after 3–4 weeks for seroconversion up to 6 months.
Results:
A total of 476 injuries were reported. Needlestick injury of fingers was the most common. Doctors were found to have the highest exposure rate (73.7%) distantly followed by nurses (19.1%). A significant number of the HCWs (125, 26.3%) vaccinated in past had hepatitis B surface antibody (anti-HBs) titers <10 mIU/mL (protection defined as anti-HBs level ≥10 mIU/ml). Only 44 sources were found to be seropositive (11 for HIV, 9 for HCV, and 24 for HBV). No seroconversion was seen in any of the exposed HCWs after 6 months.
Conclusions:
The incidence of needlestick and sharp injuries is most often encountered in emergency wards. Anti-HBs titers were suboptimal in many of the HCWs requiring a booster dose of HBV vaccination.
Keywords
Health-care workers
needlestick injury
occupational exposure
postexposure prophylaxis
splashes
underreporting
INTRODUCTION
Needlestick injuries (NSIs) as defined by the United States National Institute of Occupational Safety and Health are injuries caused by needles such as hypodermic needles, blood collection needles, intravenous (IV) stylets, and needles used to connect parts of IV delivery systems.[1] NSIs are common and to an extent inevitable in health-care workers (HCWs) during execution of their patient care services. Percutaneous exposure occurs as a result of a break in the skin caused by a needlestick or sharps contaminated with blood or body fluids. Mucocutaneous exposure occurs when body fluids come into contact with open wounds, nonintact skin such as found in eczema, or mucous membranes such as the mouth and eyes.[2] HCWs are also exposed to droplets or splashes of blood, saliva, and urine. Percutaneous injury and splashes of fluids have been recognized as a source of exposure to blood-borne pathogens such as hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV) for HCWs and responsible for a significant proportion of HBV, HCV, and HIV infections in this group.[34]
It has been estimated by the CDC that every year more than three million HCWs are exposed to blood and body fluids via sharp and mucocutaneous injuries in the United States alone with an annual estimated 6 million NSIs.[5] Due to NSIs, the risk of infections ranges from as low as 0.2–0.5% for HIV to as high as 3–10% for HCV and 40% for HBV.[6] Although contaminated needles and other contaminated sharps should not be bent, recapped, or removed, many studies have revealed that recapping being still prevalent among HCWs.[57]
There are several studies indicating that the prevalence of NSI and the risk factors associated vary among different HCW groups such as doctors and nurses depending on the place of studies like teaching institutes, hospitals, and corporate setups.[67] Occupational exposures are common in the developing world and it is believed that 40–75% of these injuries are not reported. Unreported needlestick and sharp injuries are a serious problem and stop injured HCWs from receiving postexposure prophylaxis (PEP) against HIV, which is shown to be 80% effective in preventing HIV infection in these subjects.[8] There are limited comprehensive data from India on this aspect. The present study was conducted to know the prevalence of NSI and factors responsible for NSI and also to understand the postexposure measures taken by the HCWs in a tertiary care teaching hospital in India.
MATERIALS AND METHODS
This observational prospective study was conducted at a tertiary care teaching hospital in New Delhi, the capital city of India. We analyzed the data of all the HCWs who voluntarily reported injuries by needlestick, sharps such as cannulas, broken vials and splashes on cuts, and mucous membranes by potentially infectious materials such as blood and other body fluids. Scratches with a minute or no blood oozing following the injury were classified as superficial injury and injuries penetrating through the skin or leading to bleeding wound as deep injury. As a routine practice, we administer a questionnaire to all self-reporting HCWs. The exposed HCWs were asked to fill up a self-reporting questionnaire which included information regarding the type of injury, the source of injury (known/unknown), use of personal protective equipment at the time of injury or splashes, what type of work the HCWs does, the severity of the injury, emergency/routine health care, hepatitis B vaccination status, immediate postexposure measures taken like washing of hands, status of source of exposure, and if the HCW was knowing his/her status of HIV, HBV, and HCV positivity.
We have an active PEP program with an integrated approach to prevention including awareness raising, teaching, training, protective equipment like heavy duty gloves, banning of recapping, needle cutter at every ward, sharps containers, colored-coded waste bins, vaccination as well as round the clock sharps and splashes reporting and blood testing facility based on the guidelines of the National AIDS Control Organization of India (NACO).[9] Regular classes as a part of study curriculum are conducted separately for each group of HCWs via interactive lectures, audio–visual aids and hands-on practice, especially among newly inducted staff at least once a year. The standard pro forma for tests as prescribed in the NACO guidelines for each occupational exposure was followed. Hospital infection control nurses, clinical microbiology residents, and trained technical staff were actively involved in follow-up and counseling of each exposed HCWs in our PEP program.
After taking informed written consent, serum samples from such exposed HCWs were collected along with that of patient (if known source). Screening for HIV 1 and 2 was done as per NACO guidelines.[9] Moreover, HBsAg and antibodies against HCV were done immediately by rapid tests (HBV by BioStandard Diagnostics Pvt. Ltd., Haryana, India and HCV Tri-Dot, Diagnostic Enterprises, HP, India) followed by using electrochemiluminescence immunoassay (ECLIA) kits supplied by Roche Diagnostics GmbH (Mannheim, Germany) using fully automated Cobas®6000 modular analyzer from Roche Diagnostics Ltd, Basel, Switzerland. All these tests were performed in duplicate and confirmed by immunoassay miniVIDAS, BioMerieux, Lyon, France, based on Enzyme-Linked Fluorescent Assay (ELFA principle) irrespective of the results of the preliminary screening. HCWs were also tested for hepatitis B surface antibody (anti-HBs) titers by miniVIDAS Anti-HBs Total Quick kit. Subjects with anti-HBs titer ≥10 mIU/mL were considered as responders to vaccination and <10 mIU/mL as nonresponders.[10] HCWs who got exposed to HIV seropositive patients were immediately referred to the antiretroviral therapy clinic at our hospital. For seroconversion, all HCWs under investigation were counseled and advised to get tested again after 3 weeks, 3 months, and finally after 6 months. The serum samples of patients from whom the HCWs got exposed, if known, were also tested for HIV, HBV, and HCV with viral load, if screening tests were positive. The outcomes of such exposed HCWs and rate of seroconversion were noted.
Data thus collected were entered into a computer-based spreadsheet for analysis using SPSS statistical software (version 20) (IBM Corp., NY, USA). The statistical tests applied included proportions, Student's t-test, and Chi-square tests for significance of associations.
RESULTS
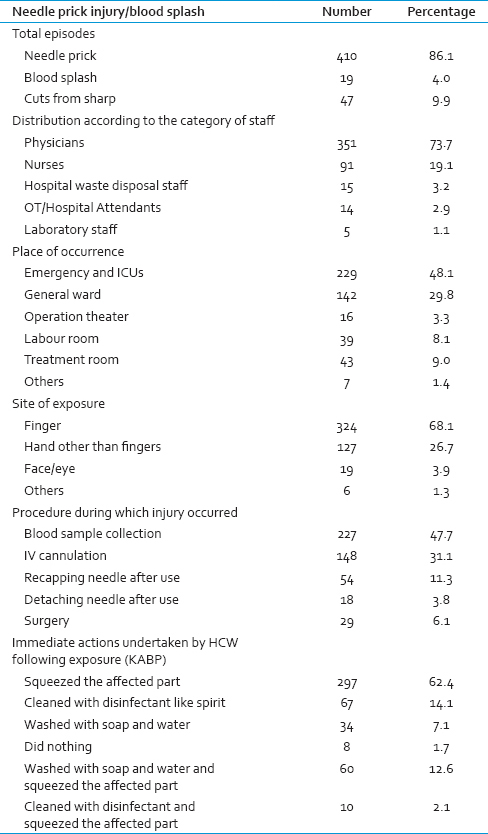
A total of 476 cases of accidental exposures were reported during the period with majority of them due to needle prick injury [Table 1]. The mean age of study group was 28.4 years (standard deviation ± 6.6) range 17–59 years, with a predominance of males (59.8%). The majority (92.2%) of the HCWs reported being right-handed and only 7.8% reported being left-handed.
Prevalence and nature of exposures
A large number of the reported incidents were doctors (351, 73.7%). Within doctors, the highest number was of resident doctors (321, 91.4%), followed by interns (26, 7.4%), and faculty members (4, 1.1%). Interestingly, only 91 (19.1%) nurses reported injuries, while 15 (3.2%) of the exposed HCWs were hospital waste disposal staff, not involved directly in patient care or surgical procedures [Table 1]. Percutaneous injuries (457, 96.0%) were more common as compared to mucocutaneous exposures (19, 4.0%). Most of the percutaneous injuries (337, 70.8%) were superficial. Most common site of injury was hands mainly fingers (94.8%). Left-hand side was most commonly involved (310, 65.1%) of which left index finger was the most common (65%) site. Most of the HCWs (384, 81.7%) reported the exposure on the same working day, while rest (92, 19.3%) reported to us on the next morning if the exposure happened during the night duties.
Factors associated with exposures
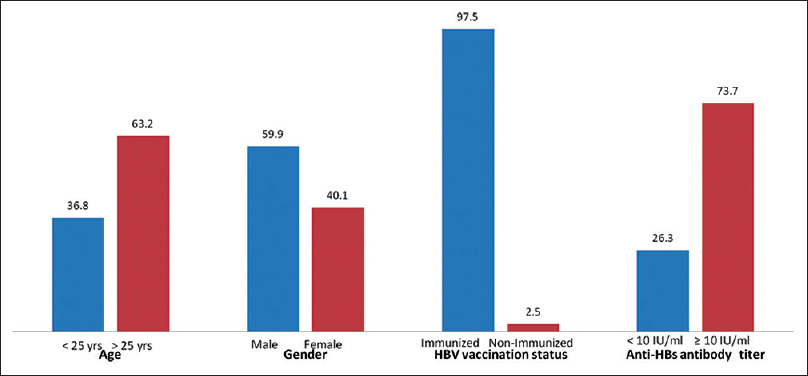
Resident doctors were more commonly exposed to percutaneous injuries. More than one-third of the NSIs were seen in young staff aged below 25 years [Figure 1]. Gender was not found to be significantly associated with injuries although the majority of the injuries were reported in males (285, 59.9%) than in females (191, 40.1%). Injuries were most commonly reported from emergency wards and Intensive Care Unit (ICU). Almost half (47.7%) of the percutaneous injuries occurred during blood sample collection and during IV cannulation (31.1%). Recapping and detachment of the needle after use were responsible for 72 injuries (15.1%) only.
- General characteristics and immune status (%) of health-care workers of AIIMS, New Delhi, who reported for healthcare-related injuries (n= 476)
Vaccination status of health-care workers
Most of the HCWs (464, 97.5%) were vaccinated against hepatitis B virus and 12 (2.5%) were not vaccinated against HBV. Most of the unvaccinated HCWs were student nurses and a few resident doctors who had joined medical profession recently. Of the vaccinated, 24 (5%) had completed three doses of the vaccine within 1 year, while 19 (3.9%) were vaccinated more than 10 years back. In 125 (26.9%) of the 464 vaccinated HCWs, anti-HBs antibody titers were <10 IU/ml, means these were nonresponders to the vaccine.
Evaluation of source
Source patient could be identified in 435 exposures only. Serological status for three major viral infections (HIV, HBV, and HCV) was unknown in 137 (31.4%) sources. However, serological status in majority of the sources (298, 68.5%) was known prior to the injury. Overall, these exposures occurred from 32 sources known to be positive for HIV, HCV, or HBV. However, after testing twelve new sources were also found to carry highly infectious viral infections [Figure 2]. Thus, the total number of these sources increased from 32 to 44, HBV from 15 to 24 (nine new cases), HIV from 10 to 11 (one new case), and HCV from 7 to 9 (two new cases). PEP either for HIV or HBV exposure was recommended in 19 HCWs (3.9%) who sustained percutaneous/splash injuries. Eleven HCWs who got exposed to HIV seropositive patients' blood were immediately referred to the antiretroviral therapy clinic. Of the 24 HCWs exposed to HBV positive sources, eight were either nonresponders to HBV vaccination or did not receive the vaccination. Therefore, they were administered hepatitis B immune globulin along with the first dose of vaccination for HBV. Remaining 16 had completed their vaccination and had protective titers of anti-HBs antibodies. The sources of nine HCWs were HCV positive patients and no immediate action was taken.
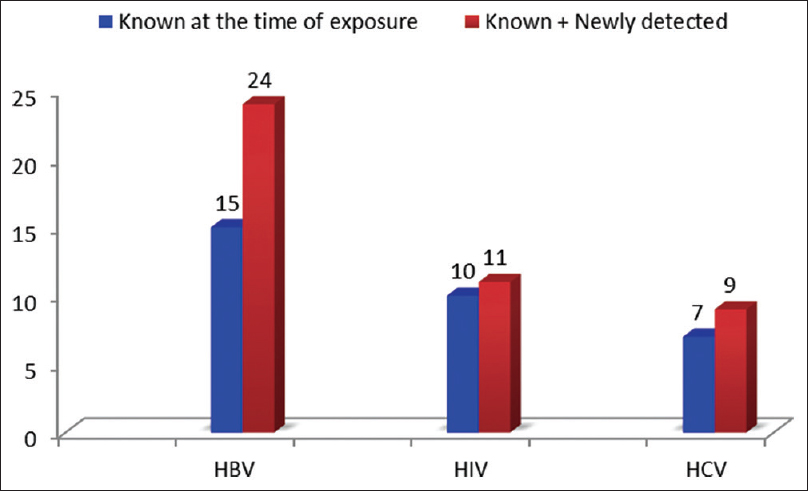
- Serological status of source patients for hepatitis B virus, hepatitis C virus, and human immunodeficiency virus infection
Knowledge, attitude, behavior, and practices of health-care workers
Insufficient level of knowledge on HIV transmission and the risks after exposure was observed expectedly more in hospital waste disposal staff as compared to physicians and nurses. Only 278 (58.4%) of the HCWs were using personal protective equipment such as gloves, masks, and gowns at the time of exposure. Cleaning the injury site with running water was the most frequently used first-aid measure in over 62.4% of the injured HCWs [Table 1]. Other measures used for immediate management included cleaning with disinfectants such as methylated spirit, hypochlorite, and soap and squeezing the site. However, 1.7% of the HCWs did not take any immediate action as the injury was superficial. Physicians most commonly took the correct measure of washing with soap and water (250, 71.2%) in comparison to nurses (44, 48.3%). This difference was statically significant (P = 0.001) [Figure 3].
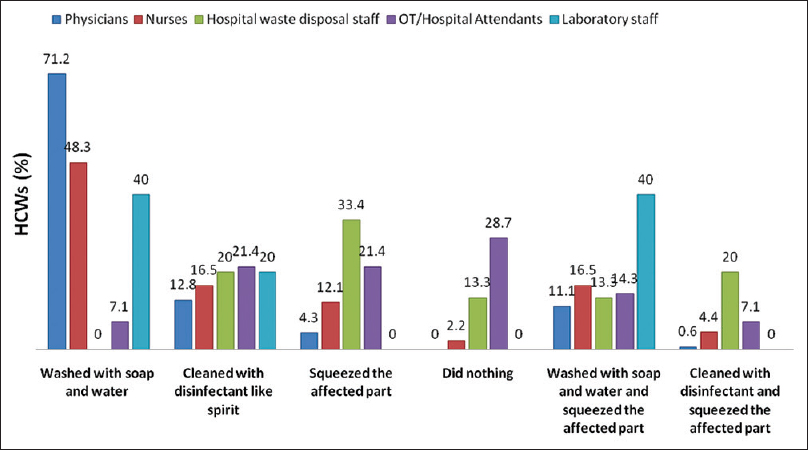
- Immediate actions undertaken by health-care workers following exposure
DISCUSSION
Occupational injuries with a needle or other sharps are common among health-care professionals. These injuries increase the risk of developing many blood-borne infectious diseases. The present study was conducted at the premier medical institute of India in New Delhi to know the prevalence of voluntarily reported the incidence of needlestick and other occupational injuries. A total of 476 incidences of exposure to blood and body fluids were reported in the study period of 3 years. This corresponds to 8.9 incidences per one hundred beds per annum. This incidence is very low when compared to 19.46 per one hundred occupied beds per annum reported in the Exposure Prevention Information Network 2011.[11] This difference may be due to lack of active surveillance or under-reporting or both since the present study is based on voluntary reporting only.
Doctors constituted the largest number (351 [73.7%]) of the reported incidents and these data correspond with several reports from India.[121314] However, other studies from India,[151617] Saudi Arabia,[18] Ireland,[19] and the USA[20] reported NSI being less frequent (19.2–28.5%) among doctors than nurses. This difference is probably because resident doctors are more commonly involved in clinical procedures in teaching institutes and hospitals like the present study setup and the work pressure at our institution, especially in emergency OPD and ICUs.
The probability of ever having a needlestick injury is inversely related to years of experience.[21] This fact was endorsed in the present study also. In our study, residents and interns aged <25 years alone constituted more than one-third (36.9%) of NSI incidences. Most of the injuries were found in newly joined academic and nonacademic junior residents. This may be due to lack of experience, handling the heavy workload of patients under pressure situations and knowledge regarding injection safety guidelines. Few other studies from India also reported similar (20.4%) prevalence rates among HCWs with experience of <10 years.[1517] NSI were more frequently reported in males (59.8%) than in females (41.2%). However, this may not be true as gender distribution among HCWs is not equal. In contrast to our findings, some studies have reported females HCWs being the most common group to sustain NSI, probably nurses.[2122]
Injuries were most commonly reported from emergency wards and ICUs (48.1%). In emergency wards, most of the time HCWs carry out the procedures on an urgent basis, and the pressure of immediate patient care increases the chances of NSI. However, many studies report operation theaters are the most common site of NSI to occur up to 53.84%.[2324] In our study, only 3.3% of NSI occurred in operation theaters. This difference could be due to the good patient–doctor ratio at this institution in operation theaters.
Recapping and postuse disposal of needles have been reported as the most common action during which HCW sustain NSI (34.0–65%).[2325] In our study, most of the injuries occurred (85%) during procedures rather than recapping (11.3%) and sharp disposal (3.7%). Contradictory results have been reported in studies conducted at Vellore (recapping 8.5%, disposal 18.6%)[26] and Goa (recapping 6.3%, disposal 31.7%).[14] This denotes increased hazard awareness among HCWs and use of safer needle disposal methods at All India Institute of Medical Sciences (AIIMS), New Delhi. In the present study, venipuncture for blood collection was the most common procedure (47.6%) during which NSI occurred. Surgical procedures like suturing contributed only 6.1% of the NSI. This is in contrast to many other studies where stitching was the most common procedure (29–46%), followed by blood sample collection (19%) responsible for NSI.[212324] This difference can be explained by better facilities and direct supervision of residents by the faculty members in a surgical procedure at AIIMS.
Of the blood-borne diseases, hepatitis B is not only the most transmissible infection but also the only one that is preventable by vaccination.[10] Anti-HBV vaccination coverage varies from 18% in Africa to 77% in Australia and New Zealand, according to the WHO estimates.[27] In our study, 97.5% of HCWs were found vaccinated against hepatitis B. This shows a significant impact of our previous study from this center only in 2008 in which vaccination coverage was found to be only 52–59% in different categories of HCWs.[28] After that study, the AIIMS administration took a decision to make the HBV vaccine available to all HCWs in 2009 onward and the positive impact of that evidence-based administrative decision is reflected in this study.
However, around one-fourth of the vaccinated individuals had anti-HBs titers <10 IU/ml, which is the protective level.[29] PEP either for HIV or HBV was taken by 3.9% of HCWs, which is comparable to other studies from India where 3–7.8% received PEP.[1323] However, this figure is low when compared to other studies where 21.6–25% took a course of PEP against HIV/AIDS, respectively.[2130] Fear of side effects has been cited as one factor in HCWs against PEP. Most important observation of the study was that no seroconversion was seen in any of the exposed HCWs when they were tested again after 3–6 months.
Cleaning the injury site with soap and water was the most frequently used first-aid measure following exposure in over 62.4% of HCWs injured. The correct method of washing the injury site was practiced by 71.3% of physicians while other HCWs showed poor knowledge about immediate action following exposure.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors wish to acknowledge the technical help of Mrs. Veena Balooni, Mrs. Shalini Singhal, and Mr. Shakeel Ahmed for technical help in carrying out the routine diagnostic tests and meticulous data recording.
REFERENCES
- Study on incidence of needle stick injury and factors associated with this problem among medical students. J Occup Health. 2003;45:172-8.
- [Google Scholar]
- Cementing sharps safety in the European union: The importance of complying with the 2010 EU council directive on sharps injury prevention. J Nurs Care. 2014;3:1-2.
- [Google Scholar]
- Evaluation of interventions to prevent needlestick injuries in health care occupations. Am J Prev Med. 2000;18(4 Suppl):90-8.
- [Google Scholar]
- Occupationally acquired infections in health care workers. Part I. Ann Intern Med. 1996;125:826-34.
- [Google Scholar]
- Needlestick injuries in the United States. Epidemiologic, economic, and quality of life issues. AAOHN J. 2005;53:117-33.
- [Google Scholar]
- Factors affecting occupational exposure to needlestick and sharps injuries among dentists in Taiwan: A nationwide survey. PLoS One. 2012;7:e34911.
- [Google Scholar]
- Centers for Disease Control and Prevention: NIOSH Publications and Products. Preventing Needlestick Injuries in Health Care Settings (2000-108). Available from: http://www.cdc.gov/niosh/docs/2000-108/
- [Google Scholar]
- Singh S, ed. Standard operative manual: Hospital infection control. New Delhi: National AIDS Control Organization, Government of India; 1999.
- Hepatitis B in health care workers: Indian scenario. J Lab Physicians. 2009;1:41-8.
- [Google Scholar]
- International Healthcare Worker Safety Center, University of Virginia. U.S. EPINet Sharps Injury and Blood and Body Fluid Exposure Surveillance Research Group. 2011. Sharps Injury Data Report. Available from: http://www.healthsystem.virginia.edu/pub/epinet/epinetdatareports.html#CitingEPINet
- [Google Scholar]
- Study on prevalence of needle stick injury among health care workers in a tertiary care hospital in New Delhi: A two-year review. Indian J Public Health. 2012;56:101-3.
- [Google Scholar]
- Risk of needle stick injuries in health care workers – A report. Indian J Med Microbiol. 2002;20:206-7.
- [Google Scholar]
- Study of needle stick injuries among health care workers at a tertiary care hospital. Indian J Public Health. 2010;54:18-20.
- [Google Scholar]
- Needle stick injury and HIV risk among health care workers in North India. Indian J Med Sci. 2011;65:371-8.
- [Google Scholar]
- Epidemiology of needle-stick injuries in Mangalore. J Evol Med Dent Sci. 2012;1:128-36.
- [Google Scholar]
- Knowledge, attitude and practices on needle-stick and sharps injuries in tertiary care cardiac hospital: A survey. Indian J Med Sci. 2010;64:396-401.
- [Google Scholar]
- Epidemiology of needlestick injuries among health care workers in a secondary care hospital in Saudi Arabia. Ann Saudi Med. 2005;25:233-8.
- [Google Scholar]
- Occupational sharps injuries in a Dublin teaching hospital. Ir Med J. 2003;96:143-5.
- [Google Scholar]
- Effects of hospital staffing and organizational climate on needlestick injuries to nurses. Am J Public Health. 2002;92:1115-9.
- [Google Scholar]
- Prevalence and factors associated with percutaneous injuries and splash exposures among health-care workers in a provincial hospital, Kenya, 2010. Pan Afr Med J. 2013;14:10.
- [Google Scholar]
- Student occupational exposure incidence: Perception versus reality. J Dent Educ. 2006;70:1081-8.
- [Google Scholar]
- Study of prevalence and response to needle stick injuries among health care workers in a tertiary care hospital in Delhi, India. Indian J Community Med. 2010;35:74-7.
- [Google Scholar]
- Brief report: Needlestick injury and inadequate post-exposure practice in medical students. J Gen Intern Med. 2005;20:419-21.
- [Google Scholar]
- Needle stick injuries among health care workers in a tertiary care hospital of India. Indian J Med Res. 2010;131:405-10.
- [Google Scholar]
- Needle stick injuries in a tertiary care hospital. Indian J Med Microbiol. 2009;27:44-7.
- [Google Scholar]
- Best infection control practices for intradermal, subcutaneous, and intramuscular needle injections. Bull World Health Organ. 2003;81:491-500.
- [Google Scholar]
- Prevalence of hepatitis B virus infection in healthcare workers of a tertiary care centre in India and their vaccination status. J Vaccines Vaccin. 2011;2:2-4.
- [Google Scholar]
- Long-term persistence of anti-HBs after vaccination against HBV: An 18 year experience in health care workers. Vaccine. 2004;22:607-10.
- [Google Scholar]
- Occupational exposure to blood and body fluids among health care workers in a teaching hospital in Mumbai, India. Indian J Community Med. 2008;33:26-30.
- [Google Scholar]





