Translate this page into:
Papillary carcinoma arising from de novo ectopic thyroid tissue within thyroglossal duct cyst: A rare case report
*Corresponding author: Upasana Mukherjee, Department of Pathology, College of Medicine and Sagore Dutta Hospital, Kolkata, West Bengal, India. mupasana@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pradhan R, Dutta A, Mondal S, Mukherjee U. Papillary carcinoma arising from de novo ectopic thyroid tissue within thyroglossal duct cyst: A rare case report. J Lab Physicians. 2024;16:561-6. doi: 10.25259/JLP_18_2024
Abstract
The most common congenital anomaly of thyroglossal duct is a thyroglossal duct cyst, but carcinoma arising from a thyroglossal duct cyst is a rare phenomenon. Carcinomas involving thyroglossal duct cysts are mostly papillary carcinomas. Definitive diagnosis of carcinomas involving thyroglossal duct cysts is done through surgical excision and subsequent histopathological examination. Most carcinomas arise de novo from ectopic thyroid tissue within thyroglossal duct cysts, but the direct spread of papillary carcinomas arising from the thyroid gland can also present themselves as carcinomas involving thyroglossal duct cysts in a minority of patients. Clinical presentation in most of the patients with carcinoma of thyroglossal duct cyst is quite similar to that of the patients with histopathologically diagnosed thyroglossal duct cyst, i.e., a painless anterior midline neck swelling with cosmetic concern and no other significant symptom(s). Careful clinical examination, imaging techniques, fine needle aspiration cytology, etc., can be helpful in indicating the presence of carcinoma preoperatively. Management of patients with thyroglossal duct cyst carcinoma involves only the Sistrunk procedure in the majority of cases. However, in a minority of patients, management by Sis trunk procedure with additional total thyroidectomy (with or without dissection of lymph nodes of the neck) and adjuvant chemo and radio-ablation therapies are needed. Here, we report a case of a 17-year-old female with papillary carcinoma involving thyroglossal duct cyst who presented with a submental swelling and was eventually managed by Sis trunk procedure, total thyroidectomy, and adjuvant therapies for optical cure. Decisions for the management of her cancer were taken through multidisciplinary interactions at tumor board meetings and by judging her surgical and therapeutic needs based on her clinical, radiological, and pathological findings.
Keywords
Papillary carcinoma
Sistrunk procedure
Thyroglossal duct cyst
Total thyroidectomy
INTRODUCTION
During 3rd week of embryonic life, the development of the thyroid gland begins with the formation of the thyroid diverticulum as a result of endodermal cell proliferation at the site of the foramen cecum within the tongue.[1] This diverticulum extends craniocaudally in the median plane by passing anterior to the hyoid bone and larynx to reach its final normal location in the anterior neck, and while doing so, it is kept attached to the base of the tongue by a rudimentary structure called the thyroglossal duct.[1] The thyroglossal duct usually does not persist after 8 weeks of intrauterine life.[1] However, if the thyroglossal duct fails to obliterate its path, it may give rise to congenital anomalies in later life, such as thyroglossal duct cysts, patent thyroglossal duct, and ectopic thyroid gland.[1] Thyroglossal duct cyst is the most common congenital anomaly associated with thyroid gland development, having a population prevalence of 7% worldwide.[2] Thyroglossal duct cysts are also the most commonly encountered midline neck swellings around the globe.[2] The majority (around 65%) of the clinically detected thyroglossal duct cysts are located at the infrahyoid level between the hyoid bone and the thyroid gland.[2] The other less common locations include suprahyoid (24%), suprasternal (13%), and intralingual (2%) locations. Clinically detectable thyroglossal duct cysts are usually painless midline anterior neck swellings that move with deglutition and tongue protrusion. Roughly around 1% of cases of detected thyroglossal duct cysts show the presence of carcinoma within them.[1] Therefore, a carcinoma involving a thyroglossal duct cyst is a rare entity, and to date, few cases of carcinoma involving thyroglossal duct cyst (approximately 300) have only been reported.[3] Here, we are reporting a case of thyroglossal duct cyst carcinoma detected in a 17-year-old female. Most of the carcinomas are of papillary type with a similar clinical presentation to that of thyroglossal duct cysts.[4] Here, we have a case of papillary carcinoma arising within the thyroglossal duct cyst. The case is reported according to the recent CARE criteria.[5]
CASE REPORT
A 17-year-old female patient had attended the surgery outpatient department (SOPD) of our institution with a painless submental swelling in the anterior neck region, which had been present since her birth and had shown a gradual increase in its size during the past 6 months before she attended SOPD. The patient did not have any remarkable medical history. On physical examination, one submental swelling slightly more lateralized toward the right side in the anterior neck region was detected, which measured 3 × 2 cm2 and moved with deglutition as well as protrusion of the tongue. The thyroid gland was found to be normal, appearing on both inspection and palpation, and no palpable lymph node was found in the neck region. Ultrasonography (USG) of the neck region and fine needle aspiration cytology (FNAC) from the swelling was advised.
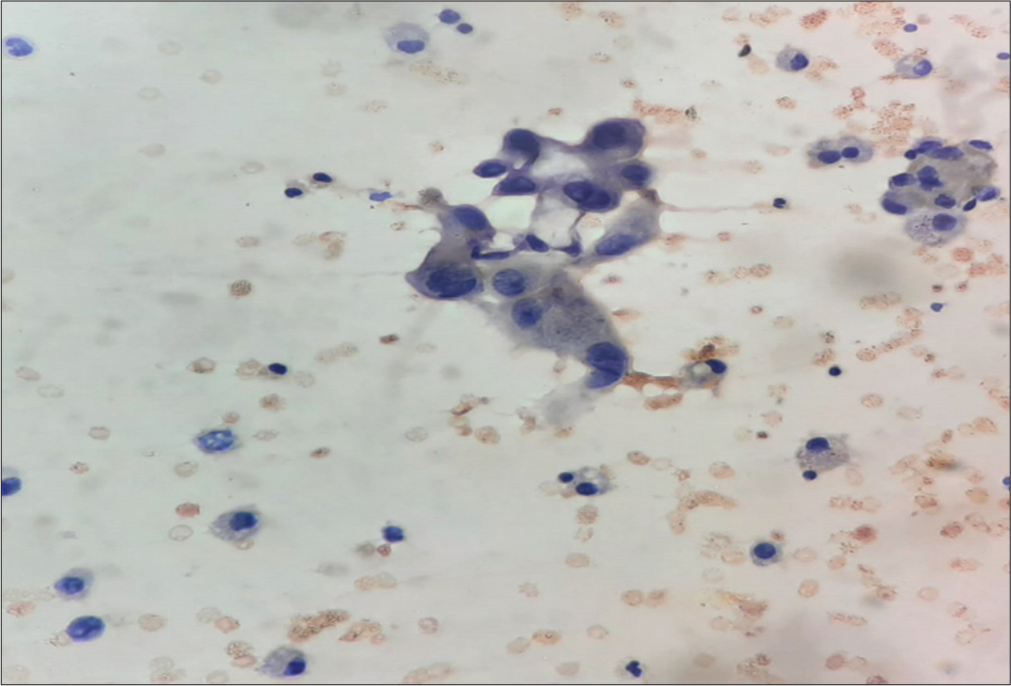
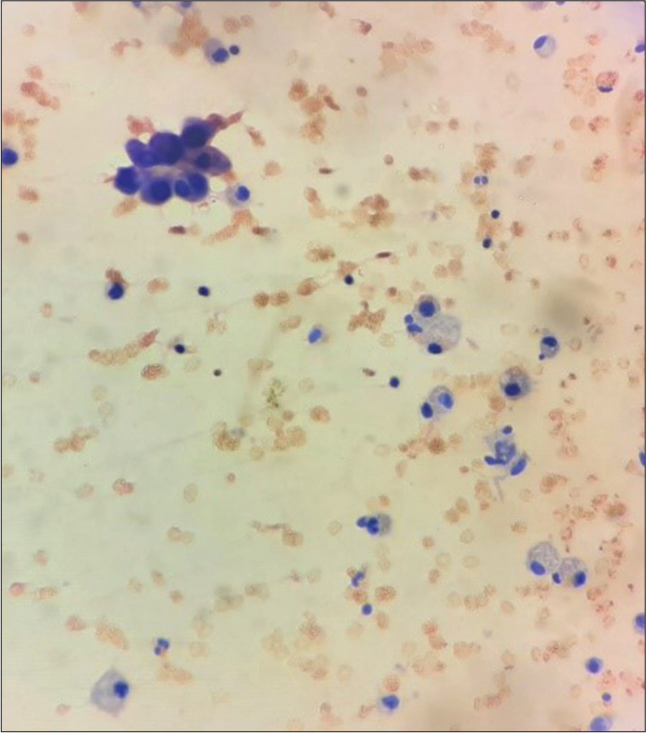
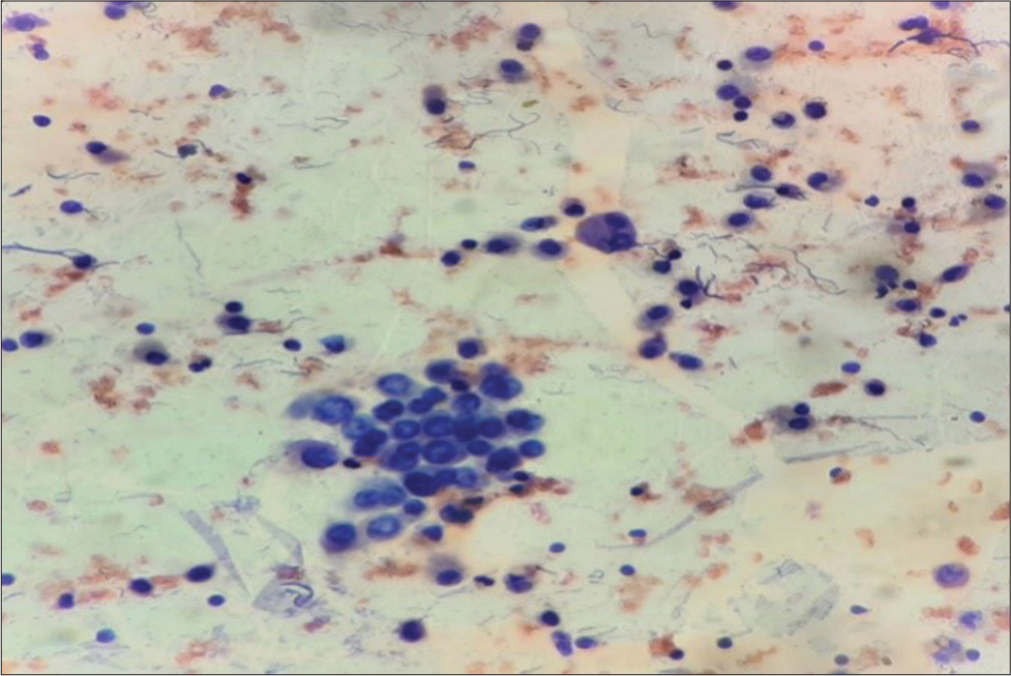
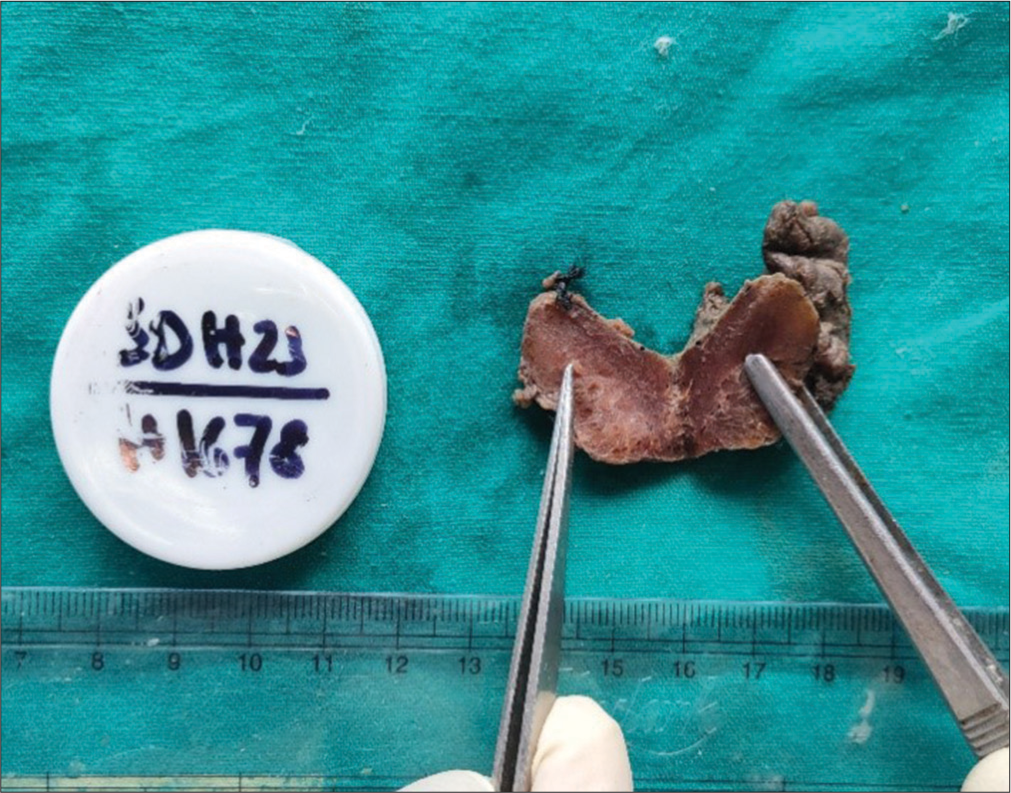
USG findings suggested the submental swelling to be a cystic lesion with doubtful presence of echogenic debris, and radiological provision differential diagnoses given were (1) a thyroglossal duct cyst, (2) a brachial cyst, and (3) a dermoid cyst. Fine needle aspiration (FNA) from the swelling was then done in the pathology department of our institution. The aspirate was a straw-coloured fluid, and the size of the swelling was slightly reduced after the procedure of FNA. On microscopic examination, the cytological smears showed cytomorphological features suggestive of thyroglossal duct cyst, but some small round cells resembling thyroid follicular epithelial cells were seen arranged in papillae-like structures along with clusters of metaplastic squamous cells showing significant cytological atypia [Figures 1-6]. The cytology report was signed out as a thyroglossal duct cyst with the advice of an urgent excisional biopsy followed by a histopathological study to rule out any underlying malignancy. The patient then underwent a Sistrunk procedure in the department of surgery of our institution, and the excised specimen was then sent to our department for histopathological examination (HPE). The excised specimen comprised a single brownish tissue piece which measured 4 × 3 × 2 cm3 and had part of hyoid bone attached to it at one end. On cutting open solid (whitish yellow), cut surfaces were seen along with a small cyst measuring 0.2 cm in maximum dimension [Figure 7]. On microscopy, there was the presence of a cyst lined by metaplastic squamous epithelium on one side and papillary thyroid carcinoma (PTC) in other areas [Figure 8]. Then, the specimen was completely embedded, and multiple sections also showed PTC originating from the de novo thyroid tissue of the thyroglossal duct cyst, and the tumor tissue had also infiltrated into the surrounding skeletal muscles and hyoid bone. Radiological and clinical workup was advised to rule out the possibility of a metastatic PTC along with any cervical lymphadenopathy. Clinical examinations and repeat USG of the neck region showed a normal thyroid gland with no cervical lymphadenopathy. Because of local infiltration of cancer into the surrounding skeletal muscles and hyoid bone in the excised specimen, the patient was considered to belong to the high-risk group of patients having carcinoma involving thyroglossal duct cyst, and therefore, prophylactic total thyroidectomy was performed on her after few weeks in the department of surgery of our institution, and the excised thyroid tissue was sent to our department for HPE. The excised thyroid specimen comprised of right lobe, left lobe, and isthmus measuring 3 × 1.5 × 0.5 cm3, 3 × 1.5 × 0.5 cm3, and 1.5 × 1 × 0.3 cm3, respectively, with the presence of a small nodule (measuring 0.8 cm in the greatest dimension) in postero-lateral part of the right lobe. On cutting open both the lobes, isthmus, and nodule, brownish homogeneous surfaces were seen [Figure 9]. Grossing of the specimen with 1 section per 1 cm was done, and the specimen was entirely embedded. Microscopic examination of all the sections (including the section from the nodule) showed normal thyroid tissue with no evidence of malignancy [Figure 10]. The patient is presently doing well, and she is under regular follow-up and post-operative drug therapy, which includes lifelong levothyroxine supplementation.
- Highly atypical cells along with cyst macrophages in the cytosmears of fluid aspirated from the thyroglossal cyst (Papanicolaou stain, ×400).
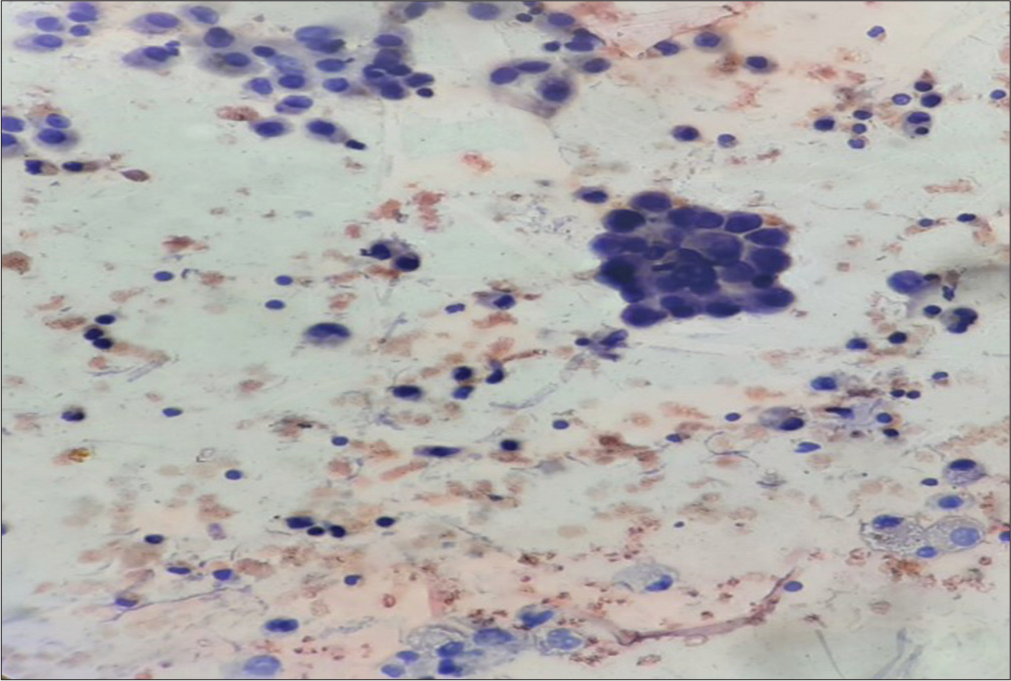
- Numerous small, atypical cells in clusters along with cyst macrophages in the cytosmears of fluid aspirated from the thyroglossal cyst (Papanicolaou stain, ×400).
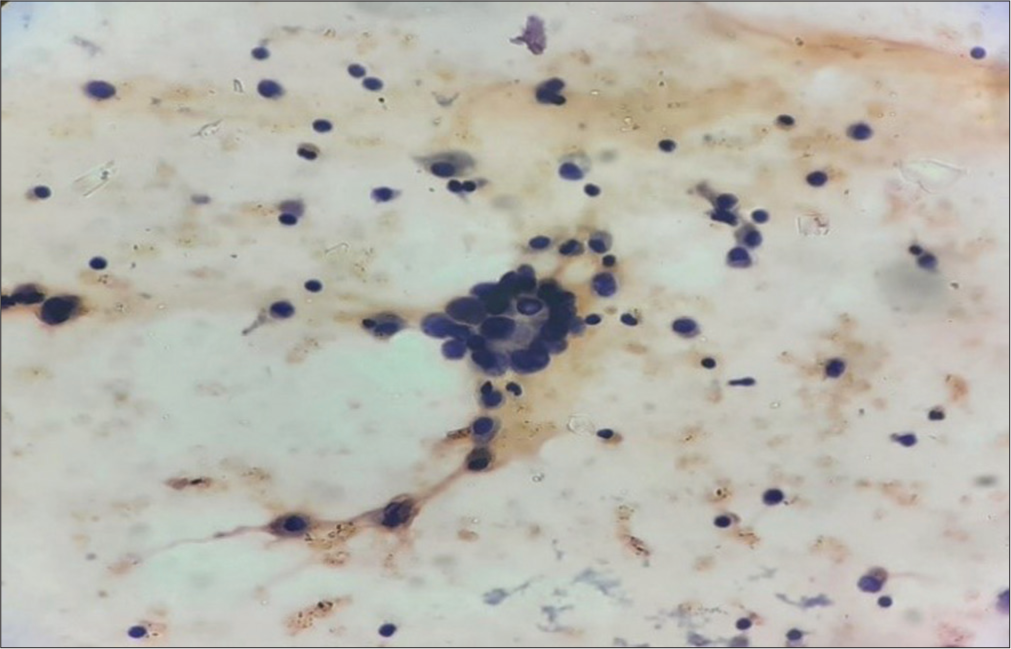
- Atypical cells with follicular arrangement along with cyst macrophages in the cytosmears of fluid aspirated from the thyroglossal cyst (Papanicolaou stain, ×400).
- Showing papillary fragments along with cyst macrophages in the cytosmears of fluid aspirated from the thyroglossal cyst (Papanicolaou stain, 400×).
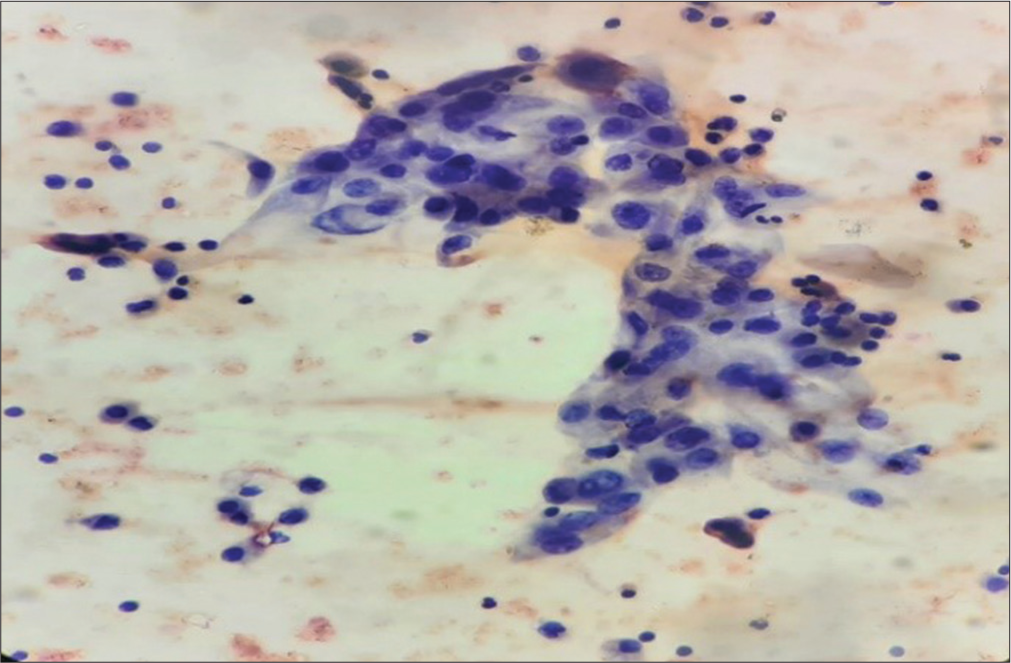
- Sheet of atypical metaplastic cells along with cyst macrophages in the cytosmears of fluid aspirated from the thyroglossal cyst (Papanicolaou stain, ×400).
- Atypical cells having ground glass nuclei along with cyst macrophages in the cytosmears of fluid aspirated from the thyroglossal cyst (Papanicolaou stain, ×400).

- Gross picture of the thyroglossal cyst with the attached hyoid bone.
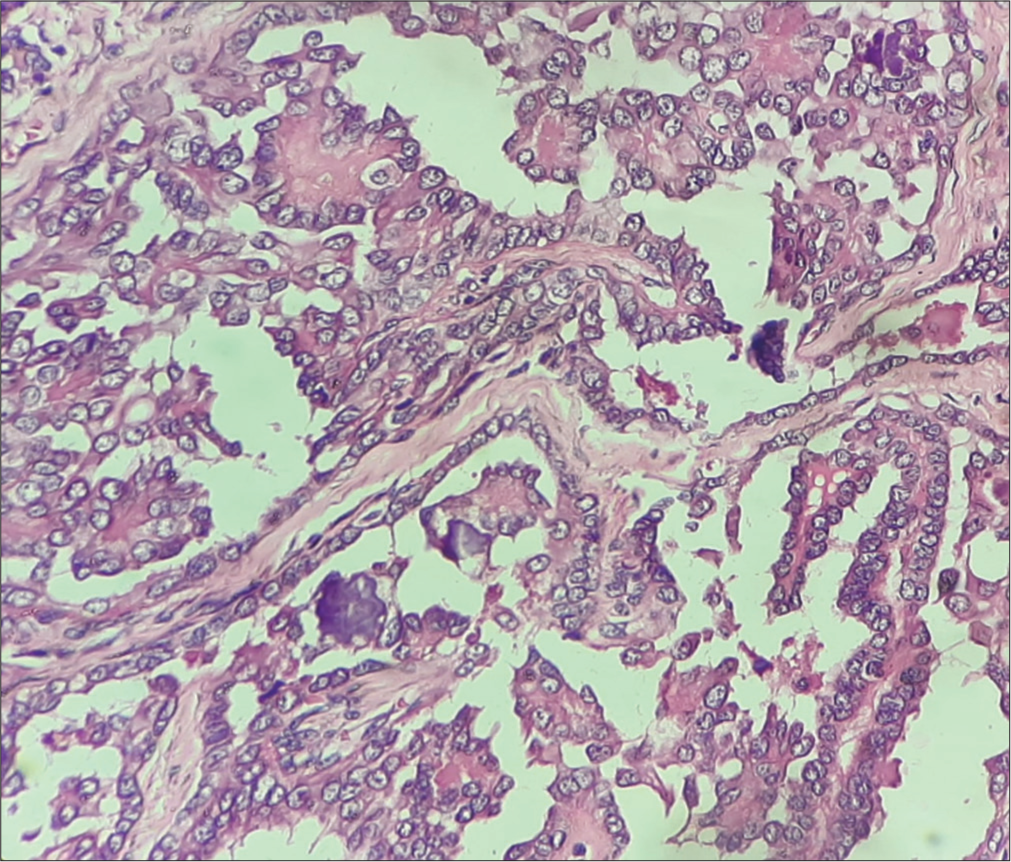
- Features of papillary carcinoma of the thyroid (micro section of the received thyroglossal cyst specimen) (Hematoxylin and eosin, ×400).
- Gross picture of total thyroidectomy specimen.
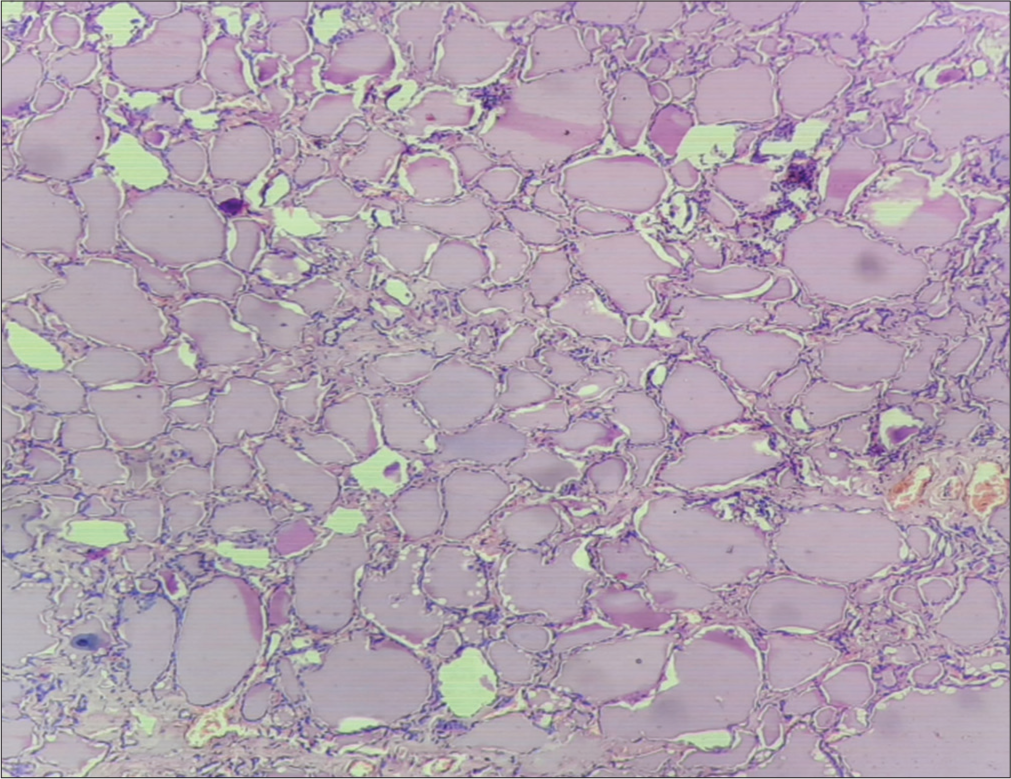
- Variable-sized thyroid follicles filled with colloid (microsection of the received total thyroidectomy specimen) (Hematoxylin and eosin, ×400).
In our case, microscopic examination of the completely embedded thyroid specimen showed no evidence of malignancy. The patient was evaluated by radionuclide iodine scan of the neck, which showed no radioiodine uptake. Due to this, the patient was not advised for any radio ablation therapy and was receiving only levothyroxine supplementation.
DISCUSSION
Carcinoma arising in thyroglossal duct cysts is a rare phenomenon seen only in approximately 1% of cases of thyroglossal duct cysts.[1] Documented case studies show an increased prevalence of carcinoma involving thyroglossal duct cyst carcinoma (TGDCC) among females in comparison to males (F: M ratio is between 1.5:1 and 2.3:1).[6] More cases have been found in adults in comparison to children, most commonly in the 4th decade of life.[6] About 4/5th (80%) cases of TGDCCs have been found to be papillary carcinomas, and the remaining cases are of mixed papillary/follicular carcinoma (8%), squamous cell carcinoma (6%), or carcinoma of another type (6%), including follicular carcinoma.[1,4] Our reported case of TGDCC was of papillary type.
In most TGDCC cases, patients usually present with midline anterior neck swelling with a cosmetic concern and no other significant symptoms [6], similar to the patients with thyroglossal duct cysts without any cancer. However, a patient with malignant transformation of thyroglossal duct cyst infrequently may also present with complaints like rapid increase in the size of neck swelling, pain, dysphagia, odynophagia, hoarseness of voice, cervical lymphadenopathy, and compressive respiratory symptoms.[7] The patient in our case report presented with a long-standing submental anterior neck swelling with a cosmetic concern.
TGDCC can originate from the ectopic thyroid tissue within the thyroglossal duct cyst of a patient, and it can also represent a metastatic deposit from a primary carcinoma involving the thyroid gland of a patient by direct spread. In most (95%) of the reported cases of TGDCC, patients have been found to be efficiently cured with the help of the Sistrunk procedure only,[7,8] suggesting that the majority of TGDCCs originate spontaneously in the ectopic thyroid tissue within the thyroglossal duct cysts of the patients.[9] However, the matter of concern in patient management lies in the fact that PTC can be multifocal in origin, and PTCs have been reported to metastasize without a primary detectable lesion in the thyroid gland.[7] Therefore, total thyroidectomy may be required along with the Sistrunk procedure on a case-to-case basis for providing optimal cure to the patients. Clinical examination: imaging techniques like USG, computed tomography (CT), magnetic resonance imaging (MRI), and FNAC can play vital roles in the pre-operative provisional diagnosis of TGDCC as well as in decision-making for total thyroidectomy in TGDCC patients by detecting the presence of suspicious thyroid gland lesions.
Detection of calcification within thyroglossal duct cyst, solid component within thyroglossal duct cyst, regional lymphadenopathy, etc., in USG of the neck, may hint toward the pre-operative diagnosis of TGDCC in a patient. In our presented case, USG findings were not suggestive of a TGDCC, though. Detection of a solid nodule within the thyroglossal duct cyst along with thickened cyst wall, calcification, margin irregularity, increased vascularity, etc., in MRI and CT scan of the neck suggests the presence of cancer within a thyroglossal duct cyst.
The diagnostic yield of FNAC most possibly depends on whether aspiration is being taken from the solid component within the thyroglossal duct cyst or not. If the malignant component within the cyst is small, the chances of cellular yield also become lower. The diagnostic accuracy of FNAC for detecting TGDCC ranges between 53% and 67%.[1] In our presented case, the FNAC report, despite being suggestive of a thyroglossal duct cyst, raised doubts toward the possibility of a TGDCC because of papillae-like arrangement of some small round cells cytomorphological resembling thyroid follicular epithelial cells and the presence of few squamous epithelial cells showing atypia suggesting metaplastic squamous cells of papillary carcinoma of thyroid tissue. Therefore, urgent excisional biopsy and histopathological study were advised.
The patient underwent the Sistrunk procedure, as this operation is done in all the preoperatively presumed or provisionally diagnosed cases of TGDCC and as this procedure has been found to be associated with an excellent prognostic value (95–100%) for the patients of TGDCCs. Removal of thyroglossal duct remnants up until the base of the tongue should be done along with en bloc surgical removal of the thyroglossal duct cyst, the middle part of the hyoid bone, during the Sistrunk procedure.[8] Total thyroidectomy is to be performed along with the Sistrunk procedure in the patients if simultaneously they also have detected lesion(s) in the thyroid gland which is suggestive of primary thyroid cancer based on clinical examination findings, other evaluations, including radio-iodine scanning and FNAC study. Dissection of the lymph nodes of the neck may also be required in these patients if they have cervical regional lymphadenopathy attributable to metastasis. Total thyroidectomy (along with or after the Sistrunk procedure) has been recommended in some studies for high-risk patients with carcinoma involving thyroglossal duct cyst who have ≥1 of the following situations: Age >45 years, tumor size >4 cm, male sex, tumor invasion to surrounding soft tissues, suspicion of cancer foci in the thyroid gland, suspicion of cervical regional lymphadenopathy due to metastasis, suspicion of distant metastatic spread, cold nodule radio-iodine thyroid scan.[8,9] After total thyroidectomy, the patient is put on thyroid hormone supplementation for a lifetime along with radio-iodine (I131) ablation therapy and thyroid-stimulating hormone suppression therapy for a suitable follow-up period. On the other hand, for low-risk patients with carcinoma involving thyroglossal duct cysts (who do not have any of the previously mentioned situations of high-risk patients), only hormone suppression therapy is recommended post-Sistrunk procedure.[8] Total thyroidectomy is rather discouraged for its associated complications in these low-risk patients as total thyroidectomy does not seem to provide any additional benefit over Sistrunk procedure for the cure of carcinoma involving thyroglossal duct cyst and survival in these patients.[10] As there was tumor invasion to the surrounding soft tissue, total thyroidectomy was performed later in our patient, considering her a high-risk patient with carcinoma involving a thyroglossal duct cyst. She is presently under regular follow-up and going through recommended post-operative drug therapies.
CONCLUSIONS
Although thyroglossal duct cyst is the most common congenital anomaly related to thyroid gland development and a common finding in the population, carcinoma involving thyroglossal duct cyst is a relatively rare entity. The majority (80%) of carcinomas involving thyroglossal duct cysts are papillary carcinomas, and they mostly arise de novo from ectopic thyroid tissue within thyroglossal duct cysts. Sistrunk procedure, total thyroidectomy, radio-iodine ablation therapy, post-operative lifelong levothyroxine supplementation, and thyroid-stimulating hormone suppression therapy are required for optimal cure in high-risk patients with carcinoma involving thyroglossal duct cyst.
Acknowledgment
We acknowledge the faculty members of the surgery department of our institution for contributing to the case of this study.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Papillary carcinoma arising from a thyroglossal duct cyst: A case report and literature review. Int J Surg Case Rep. 2022;94:107106.
- [CrossRef] [Google Scholar]
- Anatomy, head and neck, thyroid thyroglossal duct In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554494 [Last accessed on 2024 Feb 06]
- [Google Scholar]
- Papillary carcinoma within a thyroglossal duct cyst: Significance of a central solid component on ultrasound imaging. Br J Oral Maxillofac Surg. 2014;52:277-8.
- [CrossRef] [Google Scholar]
- CARE guidelines for case reports: Explanation and elaboration document. J Clin Epidemiol. 2017;89:218-35.
- [CrossRef] [Google Scholar]
- Thyroglossal duct cyst carcinoma: A systematic review of clinical features and outcomes. Otolaryngol Head Neck Surg. 2017;156:794-802.
- [CrossRef] [Google Scholar]
- Papillary carcinoma within thyroglossal duct cyst: A rare midline coexistence. Cureus. 2022;14:e31906.
- [CrossRef] [Google Scholar]
- Management of the thyroid gland in papillary carcinoma of the thyroglossal cyst: A case report. JNMA J Nepal Med Assoc. 2020;58:497-500.
- [CrossRef] [Google Scholar]
- Papillary thyroid carcinoma arising from ectopic thyroid tissue in a neck branchial cyst. SAGE Open Med Case Rep. 2023;11:2050313X231168555.
- [CrossRef] [Google Scholar]
- Management of well-differentiated thyroid carcinoma presenting within a thyroglossal duct cyst. J Surg Oncol. 2002;79:134-9. discussion 140-1
- [CrossRef] [Google Scholar]






