Translate this page into:
Recurrent Diabetic Ketoacidosis following Bariatric Surgery: The Role of Micronutrients
Address for correspondence: Mohamed Hassan Ahmed, MBBS, PhD, SCE, Department of Medicine and HIV Metabolic Clinic, Milton Keynes University Hospital NHS Foundation Trust, Eaglestone, Milton Keynes MK6 5LD, Buckinghamshire, United Kingdom (e-mail: mohamed.hassan-ahmed@mkuh.nhs.uk).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We report a case of a 29-year-old woman admitted twice to our hospital with diabetic ketoacidosis (DKA) within 45 days following her bariatric surgery. The first admission required intensive care during her postoperative days after bariatric surgery. Subsequently, she continued to report high level of ketones on a daily basis. At her second admission, she presented with all three criteria of DKA. She was treated with a standard protocol for DKA, but ketones plasma level remained high despite significant improvement in pH and glycemic control. The administration of thiamine replacement was associated with normalization of the hyperketonemia. Thiamine deficiency can be associated with bariatric surgery and can lead to high ketone level in individuals with type 1 diabetes.
Keywords
thiamine
bariatric surgery
diabetes
Background
Bariatric surgery is widely used in the treatment of morbid obesity. The benefit extends to treatment of type 2 diabetes, nonalcoholic fatty liver disease, hypertension, and dyslipidemia.[1] The Swedish Obese Subjects studies showed that bariatric procedures have a long-term effect and are associated with a significant improvement in quality of life and reduction in mortality related to cardiovascular disease and cancer.[2,3] In a systemic review and meta-analysis by Park et al, they showed that bariatric surgery was associated with an increased rate of diabetes remission.[4] In obese individuals with type 2 diabetes, bariatric surgery can be associated with remission of type 2 diabetes in around 80% cases.[2,3] The use of bariatric in type 1 diabetes is associated with decreased weight, improvement in glycated HbA1c level, and insulin dose reduction (high dose of insulin can be challenging to be administered in cases of gross obesity).[5] Different types of bariatric surgery are used, but the most commonly performed bariatric surgeries are Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy. This involves resecting part of the stomach and intestine and subsequently repositioning part of the intestine.[1-4] This can be associated with deficiency of micronutrients, including iron, folate, vitamin B1, vitamin B12, zinc, vitamin D, and calcium.[6] Therefore, individuals who have bariatric surgery performed will need dedicated and specialist nutritional support by dietician and metabolic physician to monitor and diagnose deficiencies of vitamins, trace elements, and minerals. In this case report we highlight the important of replacement of thiamine in individuals with diabetes and bariatric surgery.
Case Presentation
A 29-year-old woman presented with general malaise, abdominal pain, and hyperketonemia. She has a background of type 1 diabetes, hypothyroidism, and morbid obesity. She was diagnosed with type 1 diabetes at the age of 4 years. During adolescence, she had significant weight gain and fatigue which subsequently led to a diagnosis of hypothyroidism. Six weeks prior to presentation, she had undergone a gastric bypass surgery. Immediately after the bariatric surgery, she was admitted with severe diabetic ketoacidosis (DKA) which required intensive treatment unit (ITU) admission. Computed tomography (CT) scan of the abdomen during admission showed no evidence of postoperative complications (►Fig. 1). After discharge, she notably had significantly and persistently raised ketones: typically 3 to 5 mmol/L in the morning, which gradually improved during a day. She lost 16 kg in the 6 weeks following surgery.
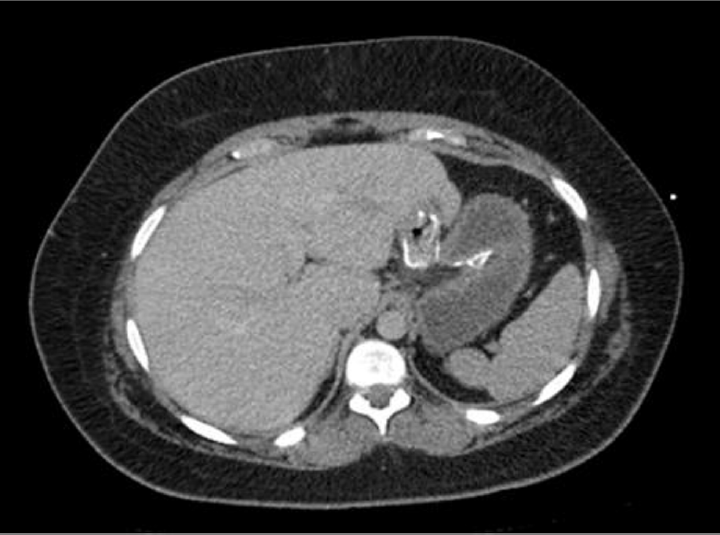
- Post gastric bypass computed tomography (CT) abdomen pelvis with contrast, demonstrating gastrojejunal anastomosis intact following bariatric surgery.
On this admission, she had worsening abdominal pain, limited oral intake, and general malaise. She reported no focal symptoms of infection. In the days prior to admission, she had noted that the previous pattern of raised morning ketones had switched to a pattern of persistent elevation throughout the day. She had continued her regular basal insulin regime and had adjusted her bolus doses appropriately for her oral intake. She was taking 8 units of tresiba in the evening, with 1 unit/10 g carbohydrate of NovaRapid with meals. Aside from insulin, she was only taking 175 µg levothyroxine once daily. On examination, she was afebrile, with respiratory rate of 16 and regular comfortable respiratory effort. Her blood pressure was 110/60 and she had a heart rate of 86. She had a Glasgow Coma Scale (GCS) of 15. Her abdomen was soft and nontender. On admission, she a capillary blood glucose of 13.3 mmol/L, ketones 4.5 mmol/L, and pH 7.267. She had a normal inflammatory marker (CRP 9.3 mg/L and WCC of 8 × 109/L) and normal renal and liver function. She was treated according to the local DKA regimen. pH, ketone, and glucose improved until they were in the normal range (►Table 1, ►Fig. 1). However, when she was transitioned onto her regular insulin regime, her ketones quickly increased again to 3 mmol/L. Empirical, thiamine 50 mg once daily supplementation began on day 2 of admission. Following starting thiamine supplementation her ketones remained controlled and remained low (< 0.5 mmol/L) (►Fig. 2). In the subsequent weeks following this admission, we monitored her ketones daily and noted these remained extremely well controlled (0.01–0.1 mmol/L). She had no further episodes of ketoacidosis or DKA in the following 4 months. The patient gave consent for publication of the case report.

- Levels of plasma glucose and ketone before and after thiamine replacement. Importantly, thiamine replacement (started on day 2) was associated with normalization of plasma ketones level, and this period is seen in the figure within those black square dots.
| Day 1 (10 a.m. admission) | Day 1 (1 p.m.) | Day 2 (6 a.m.) | Day 2 (10 p.m.) | Day 3 (3 p.m.) | |
|---|---|---|---|---|---|
| pH | 7.267 | 7.30 | 7.34 | 7.359 | 7.45 |
| HCO3 | 20.3 | 21.3 | 18.1 | 20.0 | 23.0 |
| CO2 | 6.0 | 5.5 | 4.5 | 4.8 | 4.5 |
| Na+ | 135 | 138 | 137 | 134 | 135 |
| K+ | 3.8 | 2.9 | 3.5 | 2.77 | 3.0 |
Discussion
In this case report, we have shown that thiamine replacement is associated with normalization of plasma ketones in individuals with type 1 diabetes and bariatric surgery following an episode of DKA. Importantly, Adnan et al showed that thiamine levels were decreased in individuals with type 1 and type 2 diabetes and this may be a result of increased loss of thiamine in urine.[7] The main function of thiamine is to act as cofactor of several enzymes important for carbohydrate (transketolase [TKT], pyruvate dehydrogenase, and α-ketoglutarate dehydrogenase) and amino acid (branched-chain α-keto acid dehydrogenase) metabolism.[8] Therefore, it has been suggested that individuals with diabetes will benefit from taking thiamine supplement. Importantly, thiamine deficiency can lead to high plasma ketones level in individuals with type 1 diabetes.[8] Interestingly, a clinical trial is in progress to assess whether thiamine replacement should be part of the protocol of DKA, which is expected to be completed by April 2023.[9] The half-life of thiamine is 9 to 18 days and deficiency may result from excess renal loss or excess alcohol intake. There are two methods for measurement of thiamine by the laboratory and this may require referral of the sample to the reference laboratory.[8] Therefore, we have elected to treat the patient with thiamine rather than wait for the result from reference laboratory, which may take at least 3 weeks.
Importantly, several reports have shown the association between thiamine deficiency and bariatric surgery. For instance, Tang et al showed that in cohort of 147 patients with bariatric surgery 25.7% had thiamine deficiency. Independent risk factors associated with thiamine deficiency were being African American, a larger preoperative body mass index (BMI), and self-reported repetitive episodes of nausea and vomiting.[10] Malone showed in a review article for data published within 20 years that bariatric surgery can be associated with thiamine deficiency.[11] Different case reports showed that thiamine deficiency can be severe with bariatric surgery to the extent that patients may present with Wernicke encephalopathy.[12-14]
Importantly, the level of thiamine is also noted to be low in obese individuals with intention to have bariatric surgery.[15,16] Therefore, it is plausible to suggest that in our patient different factors have contributed to the need for thiamine replacement; among them are diabetes, obesity, and bariatric surgery. Ultimately, this may have resulted in persistent high plasma ketones level since she had the bariatric surgery.
Contribution
All authors contributed equally in the manuscript.
Conflict of Interest
None declared.
References
- Bariatric surgery as potential treatment for nonalcoholic fatty liver disease: a future treatment by choice or by chance? J Obes. 2013;2013 839275
- [CrossRef] [PubMed] [Google Scholar]
- et al Swedish Obese Subjects Study. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(08):741-752.
- [Google Scholar]
- et al Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307(01):56-65.
- [CrossRef] [PubMed] [Google Scholar]
- et al Korean Research Group for Endoscopic Management of Metabolic Disorder and Obesity. Comparative efficacy of bariatric surgery in the treatment of morbid obesity and diabetes mellitus: a systematic review and network meta-analysis. Obes Surg. 2019;29(07):2180-2190.
- [CrossRef] [PubMed] [Google Scholar]
- et al Efficacy of laparoscopic sleeve gastrectomy for patient with morbid obesity and type 1 diabetes mellitus: a case report. Surg Case Rep. 2021;7(01):7.
- [CrossRef] [PubMed] [Google Scholar]
- Malnutrition as a complication of bariatric surgery—a clear and present danger? Visc Med. 2019;35(05):305-311.
- [CrossRef] [PubMed] [Google Scholar]
- Thiamine level in type I and type II diabetes mellitus patients: a comparative study focusing on hematological and biochemical evaluations. Cureus. 2020;12(05):e8027.
- [CrossRef] [Google Scholar]
- Evidence for altered thiamine metabolism in diabetes: is there a potential to oppose gluco- and lipotoxicity by rational supplementation? World J Diabetes. 2014;5(03):288-295.
- [CrossRef] [PubMed] [Google Scholar]
- Thiamine as adjunctive therapy for diabetic ketoacidosis. available at: https://clinicaltrials.gov/ct2/show/NCT03717896. Published October 24, 2018. Accessed February 18, 2021
- [Google Scholar]
- Prevalence and predictors of postoperative thiamine deficiency after vertical sleeve gastrectomy. Surg Obes Relat Dis. 2018;14(07):943-950.
- [CrossRef] [PubMed] [Google Scholar]
- Recommended nutritional supplements for bariatric surgery patients. Ann Pharmacother. 2008;42(12):1851-1858.
- [CrossRef] [PubMed] [Google Scholar]
- Wernicke's encephalopathy three weeks after sleeve gastrectomy. Surg Obes Relat Dis. 2014;10(05):992-994.
- [CrossRef] [PubMed] [Google Scholar]
- Wernicke's encephalopathy following Roux en Y gastric bypass surgery. Saudi Med J. 2015;36(12):1493-1495.
- [CrossRef] [PubMed] [Google Scholar]
- Beriberi 10 years after gastric bypass surgery—case report. Laeknabladid. 2016;102(11):497-499.
- [Google Scholar]
- Prevalence of thiamine deficiency is significant in patients undergoing primary bariatric surgery. Surg Obes Relat Dis (20):S1550-7289. 30706-1
- [Google Scholar]
- Preoperative thiamine deficiency in obese population undergoing laparoscopic bariatric surgery. Surg Obes Relat Dis. 2005;1(06):517-522. discussion 522
- [CrossRef] [PubMed] [Google Scholar]





