Translate this page into:
Thrombocytosis in children: Clinico-hematological profile from a single centre in Eastern India
Address for correspondence: Dr. Sarita Pradhan, Department of Pathology, IMS and Sum Hospital, Bhubaneswar - 751 003, Odisha, India. E-mail: dr.sarita26@gmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
BACKGROUND AND OBJECTIVE:
Thrombocytosis is not an uncommon finding in hemograms of children with an incidence of 6%–15% among hospitalized children. This study aims to determine the etiology of thrombocytosis and analyze various platelet parameters in children attending our hospital.
MATERIALS AND METHODS:
A prospective observational study was carried out in a tertiary care center in Odisha, in eastern part of India, for 6 months from July 2016 to December 2016. All children of age group 1–14 years of age attending pediatrics and other pediatric super specialty outdoors and/or admitted to indoors and whose complete blood counts (CBC) were done were included in the study. The CBC parameters such as hemoglobin, red blood cell indices, and platelet indices (platelet distribution width [PDW], mean platelet volume [MPV], platelet large cell ratio [P-LCR]) were noted.
RESULTS:
Out of 2500 hemograms done in pediatrics age group, 272 (10.8%) patients showed thrombocytosis. About 99.6% of cases were of secondary thrombocytosis. Only one case of primary thrombocytosis was encountered. The most common cause of secondary thrombocytosis was infection (39.5%) alone followed by iron deficiency anemia (14.1%). With increasing platelet counts, a decrease in MPV, P-LCR, and PDW was noted which was statistically significant (P < 0.05).
CONCLUSION:
Thrombocytosis is not rare (10.8%) in children. Secondary thrombocytosis is common and predominatly attributed to infection.
Keywords
Platelet indices
primary
secondary
thrombocytosis
Introduction
Thrombocytosis is defined as platelet count >4,00,000/ul in peripheral smear.[1] It is classified into primary/clonal or secondary according to the pathological origin. Primary thrombocytosis is classified under myeloproliferative neoplasm, which has extremely rare incidence in children (1 in 1 million). It includes essential thrombocytosis (ET), chronic myeloid leukemia (CML), primary myelofibrosis, and polycythemia vera. Secondary thrombocytosis is a reactive response to numerous conditions such as infections, inflammation, nutritional or hemolytic anemia and other hematological and nonhematological malignancies. In pediatric age group, secondary thrombocytosis remains the major category with very rare cases of primary or clonal thrombocytosis.[2]
With the advent of hematology auto-analyzers and increasing accuracy of blood cell counter, detection of thrombocytosis, especially of minor degree, has increased considerably. However, this common finding in routine hemogram often raises questions among pediatricians about the possible cause and its clinical implications. With this observation in mind, this study was carried out to assess the frequency of thrombocytosis in children as well as study the etiological causes and its correlation with the platelet parameters.
Materials and Methods
This is a prospective observational study carried out in a tertiary health center for 6 months from July 2016 to December 2016. All children of age group 1–14 years of age attending pediatrics and pediatric super specialty outdoors and indoors were included in the study. All cases with incomplete workup and repeat hemograms of same patients were excluded from the study. Routine Complete hemogram was done using 2 ml of ethylenediaminetetraacetic acid blood in 6 part differential hematology Autoanalyzer (XN-1000) and cases which showed thrombocytosis were reviewed on peripheral smear. Once it was confirmed on smear, case history, presenting signs and symptoms, history and drug history were recorded. The complete blood counts parameters such as hemoglobin, red cell indices, and platelet indices (platelet distribution width [PDW], mean platelet volume [MPV], platelet large cell ratio [P-LCR], and plateletcrit) were noted. Other relevant biochemical parameters such as C-reactive protein, erythrocyte sedimentation rate, serum iron profile, blood culture, and urine culture were also recorded as per the clinical indications in each case. Thrombocytosis was graded into mild (>500 × 103/μl–7 × 103/μl), moderate (>7 × 103/μl–9 × 103/μl), severe (>900 × 103/μl), and extreme (>1000 × 103/μl) as per Dame and Sutor[3] Etiology was determined after analyzing clinical along with relevant laboratory parameters and cases were categorized into subgroups accordingly. All the repeat hemograms of same patients were excluded from the study. The study was approved by the institutional ethical committee. Informed consent was taken from the parents of all patients included in the study.
Statistical analysis was performed on SPSS version 20. Mean, standard deviation and P value were calculated. P < 0.05 was considered statistically significant.
Results
A total of 272 children presented with thrombocytosis. Age group ranged from 1 to 14 years out of which majority were in 1–2 years age group (45.5%). Male to female ratio was 2.2:1. 70.58% children had mild thrombocytosis whereas moderate and severe thrombocytosis was seen in 25.7% and 1.5%, respectively [Table 1]. Extreme thrombocytosis was seen in 2.2% of cases. Etiology was secondary or reactive in 99.6% cases whereas only one case of primary thrombocytosis was encountered [Table 2]. Primary or clonal thrombocytosis was seen in one case of Philadelphia positive pediatric CML. No cases of ET were encountered. Etiological spectrum of secondary thrombocytosis was extremely varied. Infection was the most common cause for secondary thrombocytosis (39.5%), with the highest number attributed to respiratory tract infections alone (18.8%). Iron deficiency anemia (IDA) alone and with associated intercurrent infection was seen in 14.1% and 10.7%, respectively. Hemoglobinopathies associated with secondary thrombocytosis was seen in 8.8% of cases. Drug-induced thrombocytosis was second largest group with 15.1% cases. Out of 6 cases of extreme thrombocytosis, one case was of nephrotic syndrome with coexisting IDA, 2 cases were of postsplenectomy and three cases of severe lower respiratory tract infections.


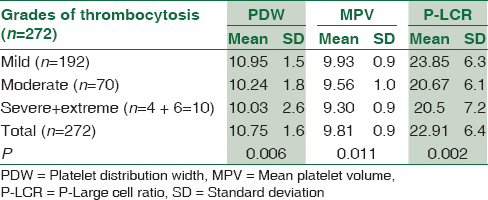
For analyzing the association of platelet indices with the severity of thrombocytosis, the cases were grouped into three categories (mild, moderate, severe + extreme) and mean value, standard deviation and P value was calculated [Table 3]. On analysis, an inverse relationship between the platelet indices and the degree of thrombocytosis was observed. With increasing platelet counts, there was a decrease in MPV which had a significant negative correlation (P < 0.05) [Table 3]. Mean PDW of children with mild and moderate thrombocytosis was 10.95fl and 10.24fl, respectively. Similar observation was seen with P-LCR where the mean P-LCR in mild and moderate thrombocytosis was 23.85% and 20.67%, respectively. In the third group of severe and extreme thrombocytosis, mean of MPV, P-LCR, and PDW were 9.3 fl, 20.5%, and 10.03, respectively.
Discussion
Thrombocytosis in children is primarily reactive or secondary and occurs as an acute phase reaction. In hospitalized children, it has been reported to have an incidence of about 6%–15%, though it is subject to variations in the definition of thrombocytosis, in study settings (hospitalized Vs outpatients), and most importantly the prevalence of causative factors such as infections, anemia, and malignancies.[3] It is often transient and secondary to underlying inflammatory conditions and reverses following treatment of the underlying cause. Frequency is higher as compared to adults due to the immaturity of innate and/or adaptive immunity and exposure to infections more frequently.[4] Primary thrombocytosis, on the other hand, is extremely rare in children. Pathomechanism of primary form is due to spontaneous production of megakaryocytic progenitors and increased sensitivity to thrombopoietin (Tpo). Whereas in secondary form, hepatic Tpo production is increased as an acute response reaction to variety of conditions[4]
In our study, thrombocytosis was found in 10.8% cases. This was in agreement to other studies by Matsubara K et al. and Dame and Sutor[23] The frequency of reactive thrombocytosis in childhood is age-dependent with the highest incidence up to 2 years of age.[2] A similar observation was noted in our study where the incidence of thrombocytosis was highest in 1–2 years age group (45.5%). Literature review shows mild increase in platelet counts up to 7,00,000/μL in 72%–86% cases, moderate and severe thrombocytosis in 6%–8% and 2%–3% of children, respectively.[3] In the present study, mild thrombocytosis was seen in 70.6%, moderate and severe thrombocytosis was seen in 25.7% and 1.5% cases, respectively, much in accordance to all previous studies.[12] Extreme thrombocytosis was seen in 2.2% cases. The incidence of newly diagnosed primary thrombocytosis in children is about 1 per 10 million, about 60 times lower than adults.[5] In our study, no case of ET was seen. One case of Philadelphia positive pediatric CML was detected. Furthermore, it was noted that with increasing age, degree of thrombocytosis was less severe, with mild cases comprising of 85% among the >10 years age group, and 65.3% among the 1–2 years age group, much in accordance to the literature review cited.[3]
A study by Dame and Sutor concluded that the most common cause for reactive thrombocytosis during childhood is (acute or chronic) bacterial or viral infections.[3] In this group, respiratory tract infection is most common followed by gastrointestinal and urinary tract infection.[67] Our study had a similar etiological spectrum with infections alone comprising 39.5% out of which respiratory tract infections was most common, followed by gastrointestinal infections and urinary tract infections.
Drug-induced thrombocytosis following intake of corticosteroids and chemotherapeutic agents like vincristine was seen in a relatively higher number of cases (15.2%) in our center. Most of these cases (39/41 cases) were of Acute Lymphoblastic Leukemia on vincristine or steroid therapy who presented with reactive thrombocytosis on multiple occasions. It has been suggested that vincristine decreases platelet utilization resulting in increased platelet life span and also increases its marrow production.[8] This high number can be attributed to the fact that this hospital is a referral center for hemato-oncology cases. Two cases of ITP on steroids also presented with rebound thrombocytosis during treatment. Corticosteroids can lead to transient thrombocytosis, by releasing stored platelets from the spleen into the blood circulation.[9] In ITP, megakaryopoiesis is accelerated as a response to immune-mediated destruction of platelets. Sometimes, during therapy, compensatory platelet overproduction in the phase of decreased or normalized platelet destruction may lead to thrombocytosis. Three cases with ITP, who developed rebound thrombocytosis following steroid treatment was reported by Yohannan et al.[10] IDA alone and with associated concurrent infections comprised 14.1% and 10.3% of secondary thrombocytosis, respectively. According to C. Sandoval, IDA remains the most common noninfectious cause of reactive thrombocytosis.[11] Hemoglobinopathies associated with reactive thrombocytosis was seen in 8.8% of cases in our study. Yadav et al. also reported 7 cases of thalassemias with reactive thrombocytosis.[12] The probable cause of relatively higher number of cases of hemoglobinopathies with also due to the fact that it is a referral center for hemoglobinopathies.
The platelet indices were compared with the degree of severity of thrombocytosis. Increase in the degree of thrombocytosis was associated with decrease in MPV, PDW, and P-LCR. Subramaniam et al. also compared the platelet indices with degree of thrombocytosis and found a weak significant negative correlation of mean MPV with degree of thrombocytosis.[13] None of the cases suffered from any kind of thromboembolic episodes.
However, this study had few limitations. The response of thrombocytosis to the treatment of underlying diseases could not be monitored in all cases, and platelet indices in reactive thrombocytosis could not be compared with the indices in primary thromocytosis (only one case in our series). A large prospective hospital-based study is already in process to see the correlation of inflammatory markers with a degree of thrombocytosis and to monitor the response of thrombocytosis and platelet indices to treatment.
Conclusion
Thrombocytosis in children is predominantly secondary and primary (clonal) thrombocytosis is extremely rare. The most common etiology of secondary thrombocytosis in children is infections and is a transient phenomenon with no major clinical implications. However, if no secondary cause is found for increased platelet count or if it persists even after treating the primary cause, a search for underlying primary thrombocytosis should be done.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Age-dependent changes in the incidence and etiology of childhood thrombocytosis. Acta Haematol. 2004;111:132-7.
- [Google Scholar]
- Thrombocytosis after pneumonia with empyema and other bacterial infections in children. Pediatr Infect Dis J. 1990;9:718-21.
- [Google Scholar]
- Reactive thrombocytosis in children with upper urinary tract infections. Acta Paediatr. 2001;90:448-9.
- [Google Scholar]
- Vincristine-induced thrombocytosis studied with 75 Se selenomethionine. Acta Haematol. 1972;47:356-60.
- [Google Scholar]
- Thrombopoietin and interleukin-6 levels in Henoch-Schönlein purpura. J Microbiol Immunol Infect. 2006;39:476-82.
- [Google Scholar]
- Thrombocytosis. Etiologic analysis of 663 patients. Clin Pediatr (Phila). 1994;33:340-3.
- [Google Scholar]
- Thrombocytosis in children with iron deficiency anemia: Series of 42 children. J Pediatr Hematol Oncol. 2002;24:593.
- [Google Scholar]
- Clinicohematological study of thrombocytosis in children. ISRN Hematol. 2014;2014:389257.
- [Google Scholar]





