Translate this page into:
Calcified Amyloid Tumor of Neck with Exuberant Giant Cell Reaction
Address for correspondence: Dr. Arghya Bandyopadhyay, E-mail: drarghyabanerjee@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Amyloidosis is a group of disorders characterized by an extracellular deposition of an abnormal amount of proteins in a variety of organs resulting from abnormal folding of protein. It typically presents as disseminated deposits. Tumor like localized presentation of amyloidosis in the absence of systemic amyloidosis is referred to as amyloidoma or amyloid tumor. Amyloidoma is the least common presentation of tissue amyloid deposition. Amyloidoma of soft tissue is again a very rare entity, especially in the neck region. Calcification and minimum giant cell reaction can occur in amyloidoma. However, extensive calcification and exuberant giant cell reaction in amyloidoma of soft tissue neck make it difficult to diagnose. In this report, we discuss such a rare case with its differential diagnoses.
Keywords
Amyloidoma
amyloidosis
giant cell
neck
INTRODUCTION
Amyloidoma is defined as a localized, solitary tumor like deposit of amyloid without any evidence of systemic amyloidosis.[1] Amyloidoma of soft tissue is a rare entity especially in the neck region.[23] Calcification and giant cell reaction can rarely occur in amyloidoma,[2] and it causes a great diagnostic difficulty. Herein, we present an unusual case of solitary soft tissue amyloidoma of neck with calcification and exuberant giant cell reaction.
CASE REPORT
A man of 48 years presented with a mass in the right side of the neck without any systemic complain. Initially, the lesion was a small nodule and then gradually enlarged to its present size for last 4 years. Patient gave a history of tuberculosis 5 years back which was treated completely. General and systemic examinations of the patient were unremarkable excepting the presence of large, firm mass measuring 7 × 5 × 2 cm in the right side of the neck, which was not fixed to underlying structures. The patient underwent fine needle aspiration cytology (FNAC) examination of the lesion in a private clinic before. In FNAC, it was suggested as granulomatous lesion probably due to tuberculosis. Plain and contrast computed tomography scan of neck revealed a large enhancing calcified well-circumscribed solid mass lesion (75 × 65 mm) mm on the right side deep to sterno-cleido-mastoid muscle extending from C2 to D2 vertebra with mass effect over right lobe of thyroid and right sided great vessels [Figure 1a and b]. The consultant favored the lesion as neoplastic and excision biopsy was done. On gross examination, the mass was large in size (7 × 5 × 3 cm), firm in consistency, having a smooth, waxy, brownish-yellow colored surface. The mass was un-encapsulated, but fairly well-circumscribed [Figure 2]. The histopathological examination showed extracellular deposit of eosinophilic amorphous material in the soft tissue most strikingly around the blood vessels. There was exuberant proliferation of foreign-body type giant cells around the deposit. Large areas of dystrophic calcification and lympho-plasmacytic infiltration were noted. Initially, localized amyloidosis was suspected. Several special stains such as Von Kossa, periodic acid-Schiff (PAS), Van Gieson and Congo red stain were performed. The calcified areas were positive for Von Kossa stain. The amorphous material was weakly positive for PAS but negative for Van Gieson stain. The material was intensely congophilic and showed a characteristic “apple-green” birefringence of amyloid [Figure 3a–d]. The Congo red staining was resistant to permanganate pretreatment suggesting AL (amyloid light chain)-type amyloid.[4] A final diagnosis of amyloidoma of soft tissue was rendered. Further investigations to search systemic involvement such as serum protein electrophoresis, urine electrophoresis, kidney function test, liver function test were done and the reports were found within the normal limits. The patient was kept under regular follow-up. There was no evidence of disease progression for last 1-year.
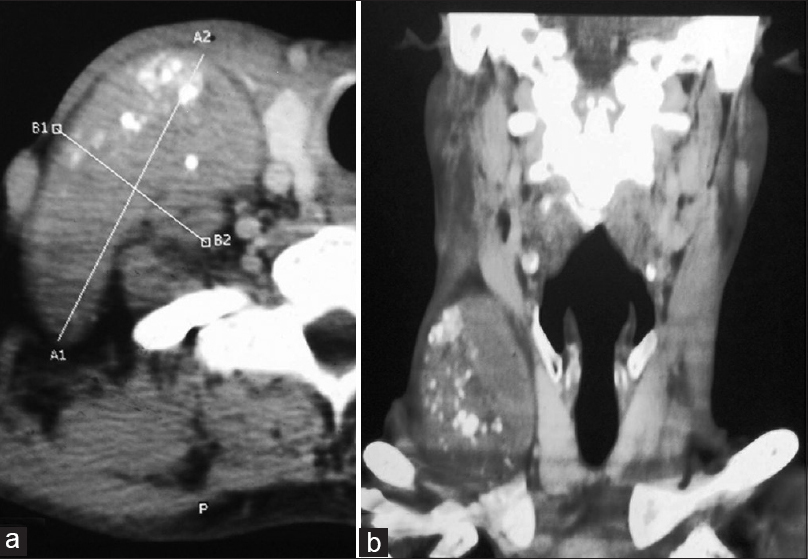
- (a and b) Computed tomography with contrast of neck showing a large enhancing well circumscribed solid calcified mass lesion on right side of neck extending from C2 to D2 vertebral level
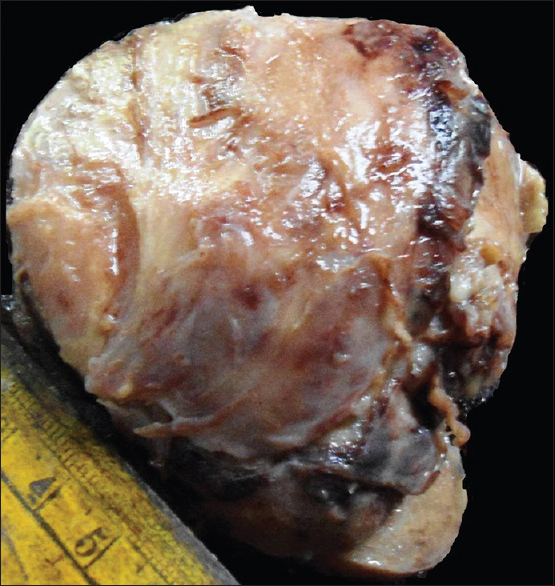
- Gross appearance of amyloidoma, showing well circumscribed but un-encapsulated brown colored tumor mass
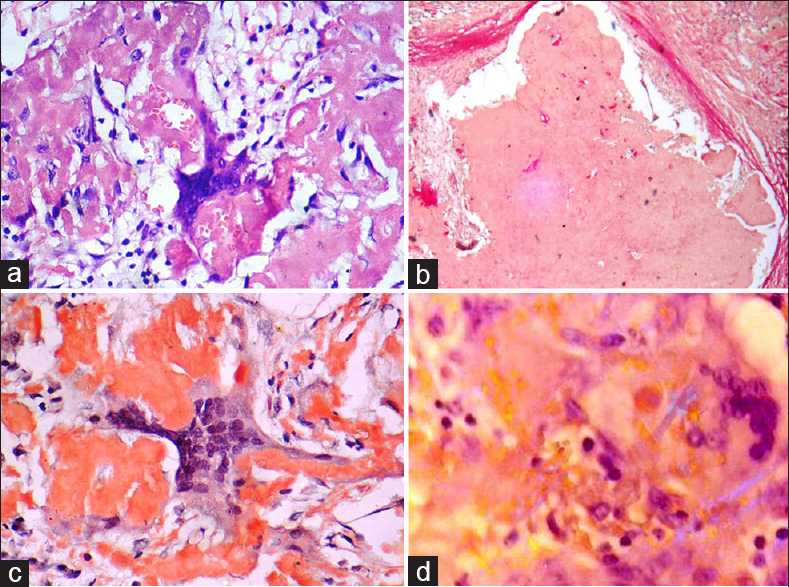
- (a) The section showing amorphous eosinophilic deposit of amyloid and exuberant giant cell reaction around the deposit (H and E, ×400). (b) The extracellular amyloid deposit show negative staining with Van Gieson stain (×100). (c) Extra cellular amyloid material staining positively with Congo red (×400). (d) The deposit is showing faint apple-green birefringence on polarization (×400)
DISCUSSION
Amyloidoma have been reported in many anatomic sites including the respiratory, genitourinary, gastrointestinal tracts, central nervous system, skin, bone, heart, lymph node and breast. However, it rarely affects the soft tissues of the neck. In head-neck region, larynx is the most common site for amyloid deposition.[25678]
The pathological diagnosis of amyloidoma of neck is difficult especially if there is florid giant cell reaction. In most of the reported cases, the initial diagnosis was of a foreign-body granulomatous reaction. Few other conditions such as tumoral calcinosis, tophaceous pseudogout and giant cell tumor of soft tissue may morphologically mimic amyloidoma.[2789] The present case was misdiagnosed in FNAC as granulomatous lymphadenitis favouring tuberculosis, as there was past history of tuberculosis. However on histopathology, the eosinophilic amorphous material was congophilic and showed faint apple-green birefringence on polorization, which established the diagnosis of amyloidoma.
The distinction between AL (amyloid light chain) and AA (amyloid associated) fibrils in amyloidoma is important. Krishnan et al.[5] found that 10 of their 14 patient of soft tissue amyloidoma had AL fibrils that constituted a primary amyloidoma and of these 80% subsequently developed a lymphocytic or plasmacytic malignant neoplasm. Hence the evaluation for systemic involvement is essential for such case. In our case, there was a history of tuberculosis so it was expected that the lesion would be of AA type, but in contrast the deposit was found to be AL-type amyloid. A similar report was published by Mukhopadhyay et al.[2] that occurred in leg.
The pathogenesis of AL amyloidosis is poorly understood. It is hypothesized that localized AL amyloidoma occurs from a small plasma cell clone, which is formed after prolonged antigen stimulation. The amyloidogenic light chains produced by the plasma cells are modified within the giant cells to form insoluble fibrils. Some investigators opine that the process can be classified as low-grade B-cell lympho-proliferative disorder, but others suggested that the lesion is possibly burnt out plasmacytoma.[10] However, this is a truly neoplastic condition, and the treatment of choice seems to be local radical excision with long-term follow-up.[10]
Finally, to conclude, although rare, amyloidoma should be considered in the differential diagnosis of neck masses whenever any extracellular amorphous material deposit is found, and special stains should be done for confirmation. Extensive giant cell reaction and calcification may lead to misdiagnosis. Pathologists should be aware of this entity in the differential diagnosis of giant rich lesions of soft tissue.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Localized amyloidosis of the head and neck and upper aerodigestive and lower respiratory tracts. Ann Otol Rhinol Laryngol. 1984;93:374-9.
- [Google Scholar]
- Recurrent amyloidoma of soft tissue with exuberant giant cell reaction. Arch Pathol Lab Med. 2003;127:1609-11.
- [Google Scholar]
- The potassium permanganate method. A reliable method for differentiating amyloid AA from other forms of amyloid in routine laboratory practice. Am J Pathol. 1979;97:43-58.
- [Google Scholar]
- Tumoral presentation of amyloidosis (amyloidomas) in soft tissues. A report of 14 cases. Am J Clin Pathol. 1993;100:135-44.
- [Google Scholar]
- Amyloidoma of bone, a plasma cell/plasmacytoid neoplasm. Report of three cases and review of the literature. Am J Surg Pathol. 1997;21:179-86.
- [Google Scholar]
- Rosai and Ackerman's Surgical Pathology. (10th ed). Missouri: Mosby; 2011. p. :2106-92.
- [Google Scholar]





