Translate this page into:
Deadly hospital-acquired Chryseobacterium indologenes sepsis in a postpartum patient
*Corresponding author: Sheetal Verma, Department of Microbiology, King George’s Medical University, Lucknow, Uttar Pradesh, India. dr.sheetal2001@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Verma A, Verma S, Venkatesh V. Deadly hospital-acquired Chryseobacterium indologenes sepsis in a postpartum patient. J Lab Physicians. 2024;16:215-8. doi: 10.25259/JLP-16-215-(1881)
Abstract
Chryseobacterium indologenes is an emerging multidrug-resistant Gram-negative bacillus associated with severe nosocomial infections. We present a case of a 27-year-old postpartum woman who developed a life-threatening Chryseobacterium indologenes sepsis following a stillbirth. Despite prompt diagnosis and intensive care management, the patient’s condition deteriorated rapidly and was fatal. Thus, highlighting the challenges posed by the multidrug-resistant nature of this pathogen and the limited treatment options available.
Keywords
Chryseobacterium indologenes
Nosocomial infection
Multidrug resistance
Sepsis
Postpartum
INTRODUCTION
Chryseobacterium indologenes, a member of the genus Chryseobacterium, is a Gram-negative bacillus commonly found in soil and water environments.[1] While it is typically considered a rare human pathogen, its ability to cause severe nosocomial infections, especially in immunocompromised and critically ill patients, is of growing concern. Chryseobacterium indologenes infections are associated with a multidrug-resistant pattern, making treatment selection challenging.[2] Limited options, such as fluoroquinolones, trimethoprim- sulfamethoxazole, and rifampin, exist for the management of this pathogen, further complicating clinical decision-making.[2] After an extensive search of the literature, we find an increasing trend of prevalence of C. indologenes infection after the introduction of colistin and tigecycline usage.
CASE REPORT
A 27-year-old woman presented to the emergency Department of Obstetrics and Gynecology with altered sensorium, fever, abdominal pain, generalized edema, and malaise for five days following a stillbirth with normal vaginal mode of delivery. On day two postpartum, she developed fever, chills, and rigor, along with stabbing abdominal pain and malaise. Referred to a higher center on day five postpartum, she exhibited disorientation, high-grade pallor, and icterus. Initial vital signs revealed fever (101°F), tachycardia (110 beats/min), hypotension (80/54 mm Hg), tachypnea (28 breaths/min), and severe anemia (hemoglobin 3.8 g/dL). Laboratory investigations showed leukocytosis (18,000/µL) and elevated C-reactive protein (59 mg/L). Microbiological identification, using two sets of automated blood culture, both sets revealed the growth of C. indologenes on sheep blood agar and MacConkey agar. The colonies exhibited characteristic features, including yellow coloration, low convexity, smooth texture, and non-hemolytic properties [Figure 1]. Gram staining confirmed the presence of Gram-negative bacilli. Biochemical tests (indole: positive, methyl red: negative, Voges-Proskauer’s: negative, triple sugar iron (TSI) glucose was utilized with gas production, and flexirubin pigment was detected with 40% H2SO4) and matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) confirmed the organism as Chryseobacterium indologenes [Figure 2]. Antimicrobial susceptibility testing demonstrated that the organism was susceptible to minocycline with minimum inhibitory concentration <1 (µg/mL) and tetracycline and resistant to all other antibiotics by disc diffusion test [Table 1] and the VITEK 2 system (Biomérieux India Pvt., Ltd., New Delhi, India).
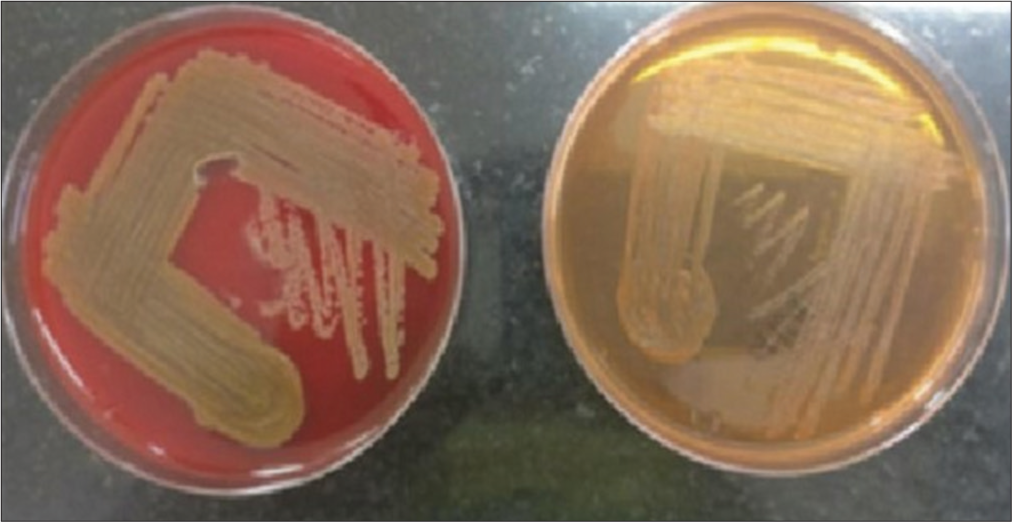
- Illustrates the yellow-orange pigment production of the Chryseobacterium indologenes isolate. The colonies on sheep blood agar exhibited a distinct yellow coloration, measuring approximately 2-3 mm in diameter. This characteristic pigment production is a key identifying feature of Chryseobacterium indologenes.
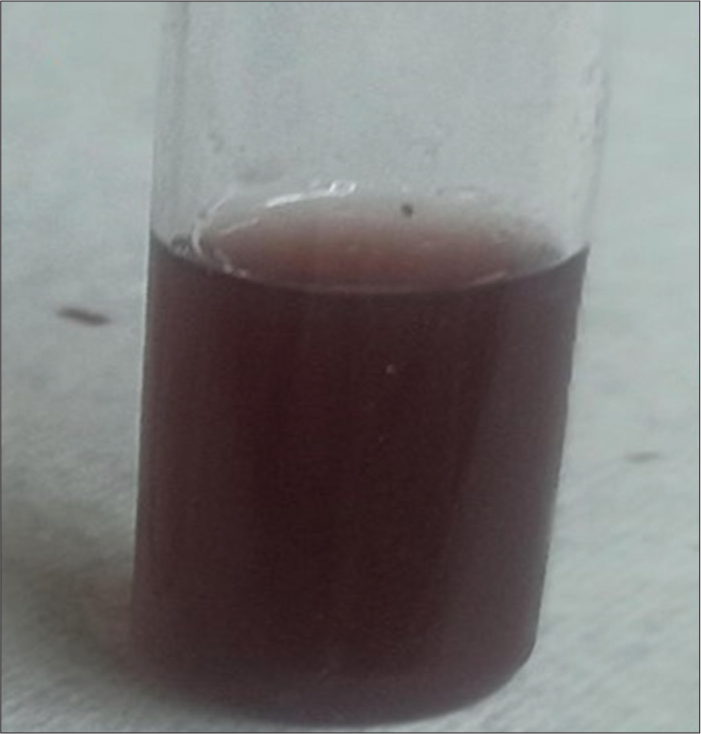
- Demonstrates the flexirubin pigment production of the Chryseobacterium indologenes isolate.The presence of flexirubin pigment was detected using 40% sulphuric acid H2SO4.
| Antibiotic | Zone size (mm) | Susceptibility |
|---|---|---|
| Meropenem (10 µg) | <19 | Resistant |
| Ertapenem (10 µg) | <18 | Resistant |
| Imipenem (10 µg) | <19 | Resistant |
| Aztreonam (30 µg) | <17 | Resistant |
| Amikacin (30 µg) | <14 | Resistant |
| Gentamicin (10 µg) | <12 | Resistant |
| Tobramycin (10 µg) | <12 | Resistant |
| Ciprofloxacin (5 µg) | 22 | Intermediate |
| Levofloxacin (5 µg) | 18 | Intermediate |
| Cefozolin (30 µg) | <14 | Resistant |
| Cefepime (30 µg) | <18 | Resistant |
| Ceftriaxone (30 µg) | <19 | Resistant |
| Minocycline (30 µg) | 20 | Sensitive |
| Tetracycline (30 µg) | 16 | Sensitive |
| Amoxicillin-clavulanate (20/10 µg) |
<13 | Resistant |
| Piperacillin-tazobactam (100/10 µg) |
<17 | Resistant |
| Trimethoprim and sulfamethoxazole (1.25/23.75 µg) |
14 | Intermediate |
| Colistin (MIC)* | >4 µg/mL | Resistant |
The table displays the zones of inhibition for various antibiotics tested, indicating the susceptibility or resistance of the isolates. It provides valuable information on the antibiotic profile of the C. indologenesstrain in this case, which showed resistance to multiple antibiotics. C. indologenes: Chryseobacterium indologenes, MIC*: Minimum inhibitory concentration
Initial treatment with meropenem and colistin, based on empirical therapy, was modified based on antimicrobial susceptibility results that was a combination therapy with minocycline and ciprofloxacin. However, due to the multidrug-resistant nature of Chryseobacterium indologenes, treatment options were limited. The organism was susceptible only to minocycline and tetracycline, further narrowing the therapeutic choices. Despite aggressive management in the intensive care unit, the patient’s condition rapidly deteriorated, and she succumbed to the infection.
DISCUSSION
Chryseobacterium indologenes, a member of the genus Chryseobacterium, is an emerging nosocomial pathogen that has been associated with severe infections, particularly in immunocompromised and critically ill patients.[3] Despite being considered a rare human pathogen, the incidence of Chryseobacterium indologenes infections have been increasing, and its multidrug-resistant pattern poses a significant challenge in clinical management.
In this case, the patient presented with symptoms of altered sensorium, fever, abdominal pain, generalized edema, and malaise, which are consistent with systemic infection. The isolation of Chryseobacterium indologenes from blood cultures indicated a bloodstream infection, which is a serious and potentially life-threatening condition; the source of infection in this case was probably during delivery time. The multidrug-resistant nature of the organism further complicated the treatment approach.[4] Chryseobacterium indologenes infections are commonly associated with healthcare settings, and have been linked to the use of invasive medical devices, such as intravascular catheters, endotracheal tubes, and prosthetic devices.[5] Contaminated water systems and wet surfaces in hospitals can serve as reservoirs for this bacterium, leading to colonization and subsequent infection in susceptible individuals.[6,7]
The limited treatment options for Chryseobacterium indologenes infections pose a significant therapeutic challenge. This bacterium is intrinsically resistant to aminoglycosides, and its chromosomal metallo-beta-lactamases contribute to resistance against beta-lactam antibiotics.[8] In this case, the isolate demonstrated resistance to meropenem and colistin, which are often used as empirical therapies for Gram-negative infections. The organism was only susceptible to minocycline and tetracycline, further narrowing the available treatment choices.
The emergence of multidrug resistance in Chryseobacterium indologenes is a growing concern. It has been observed that the increased usage of colistin and tigecycline, which are considered last-resort antibiotics for multidrug-resistant infections, has contributed to the selection pressure and subsequent rise in C.indologenes infections.[9] This highlights the need for judicious use of antibiotics and strict infection control measures to prevent the spread of multidrug-resistant strains in healthcare settings.
There is currently a lack of established recommendations for the management of Chryseobacterium. indologenes infections. Treatment options are often based on in vitro susceptibility testing, but the clinical efficacy of available antibiotics against this pathogen remains limited.[10] Further, research is needed to identify new therapeutic strategies and develop effective treatment regimens for these infections.
CONCLUSIONS
Chryseobacterium indologenes is a challenging multidrug-resistant pathogen associated with severe nosocomial infections. Our case underscores the importance of early identification, appropriate antimicrobial therapy, and stringent infection control measures to combat the rising incidence and associated mortality of Chryseobacterium indologenes infections.
Research quality and ethics statement
The authors followed applicable EQUATOR Network guidelines (http://www.equator-network.org/), notably the CARE guideline, during the conduct of this report. Declaration of patient consent: The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Lumboperitonial shunt infection due to Chryseobacterium indologenes. Pediatr Infect Dis J. 2007;26:657-9.
- [CrossRef] [PubMed] [Google Scholar]
- Chryseobacterium indologenes non-catheter-related bacteremia in a patient with a solid tumor. J Clin Microbiol. 2005;43:2021-3.
- [CrossRef] [PubMed] [Google Scholar]
- Chryseobacterium spp-associated bacteraemia in a haemodialysis patient: A diagnostic challenge. BMJ Case Rep. 2019;12:e232000.
- [CrossRef] [PubMed] [Google Scholar]
- Chryseobacterium indologenes An emerging infection in the USA. BMJ Case Rep. 2016;2016:232000.
- [CrossRef] [PubMed] [Google Scholar]
- Chryseobacterium indologenes infection in a newborn: A case report. J Med Case Rep. 2011;5:10.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and microbiological characteristics of Chryseobacterium indologenes bacteremia. J Microbiol Immunol Infect. 2010;43:498-505.
- [CrossRef] [PubMed] [Google Scholar]
- Chryseobacterium meningosepticum in a parapneumonic effusion in a chronic kidney disease patient on hemodialysis. Hemodial Int. 2014;18:835-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical correlation and antimicrobial susceptibility pattern of Chryseobacterium spp.: A three year prospective study. Intractable Rare Dis Res. 2021;10:37-41.
- [CrossRef] [PubMed] [Google Scholar]
- Chryseobacterium indolegenes infection in a patient with chronic obstructive pulmonary disease. Drug Discov Ther. 2017;11:165-7.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and microbiological characteristics of Chryseobacterium indologenes bacteremia. J Microbiol Immunol Infect. 2016;49:198-204.
- [Google Scholar]






