Translate this page into:
Evaluation of human epididymis protein 4, risk of ovarian malignancy algorithm, and risk of malignancy index efficiency for ameliorating sensitivity and specificity for differentiating benign from malignant adnexal masses
*Corresponding author: Sonia Chawla, MSc, PhD, Department of Biochemistry, Guru Gobind Singh Medical College and Hospital, Faridkot 151203, Punjab, India soniankushkamra@gmail.com
How to cite this article: Chawla S, Goyal G, Grover S, Nibhoria S, Kaur J. Evaluation of human epididymis protein 4, risk of ovarian malignancy algorithm, and risk of malignancy index efficiency for ameliorating sensitivity and specificity for differentiating benign from malignant adnexal masses. J Lab Physicians. 2024;16:36-43. doi: 10.1055/s-0043-1775590
Abstract
Objectives:
Inadequacy of effective sensitive and specific screening modalities results in late-stage diagnosis of ovarian cancer. Cancer Antigen-125 (CA-125) individually possesses limited specificity for differentiating adnexal masses. The present study aimed to evaluate the Human Epididymis Protein 4 (HE4), Risk of Ovarian Malignancy Algorithm (ROMA), and Risk of Malignancy Index (RMI) for ameliorating sensitivity and specificity for differentiating benign from malignant adnexal masses.
Materials and Methods:
This study was conducted on 96 preoperative women with suspected adnexal mass (patients) and 48 healthy females without adnexal mass (controls) for the duration of 2 years. Both study participants were divided into two groups, pre-and postmenopausal. CA-125 and HE4 were done using commercially available kits. ROMA% and RMI were calculated. We validated their performances using histopathology as the gold standard. The statistical analysis was done using SPSS 21, Kruskal–Wallis, and Tukey’s tests. The best cutoff points to best values of sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were also evaluated.
Statistical Analysis:
The statistical analysis was done using SPSS 21. All study subjects were categorized based on menopausal status and final pathology of masses based on biopsy results into pre-and post-M and benign, malignant, and borderline masses groups, respectively. Comparisons were made between these by the Kruskal-Wallis test along with Tukey's test. For all of the statistical comparisons, a level of p < 0.05 was accepted as statistically significant and standard error was also calculated.
Results:
For differentiating benign from malignant masses in the premenopausal group, the sensitivity, specificity, PPV, NPV, and area under the curve (AUC) were 93.7%, 78.3%, 65.2%, 96.6%, 0.892 for CA-125; 87.5%, 83.7%, 70%, 93.9%, 0.926 for HE4; 93.7%, 70.2%, 57.6%, 96.2%, 0.927 for ROMA; and 68.7%, 86.4%, 68.7%, 86.5%, 0.916 for RMI. While in the postmenopausal group, the sensitivity, specificity, PPV, NPV, and AUC were 92.3%, 76.4%, 85.7%, 86.6%, 0.907 for CA-125; 78.5%, 94%, 95.6%, 80%, 0.955 for HE4; 92.3%, 94.1%, 96%, 88.8%, 0.968 for ROMA; and 88.4%, 88.2%, 92%, 83.3%, 0.943 for RMI.
Conclusion:
For differentiating benign from malignant masses more specifically in women with a suspected adnexal mass, ROMA and HE4 appear to be more effective than CA-125.
Keywords
CA-125
HE4
ROMA
RMI
premenopausal
postmenopausal
INTRODUCTION
Ovarian cancer (OC) is fatal amid gynecologic malignancies and is a culprit behind the silent killing of many women across the globe because of its silent and symptomless nature of development during the onset of the disease. Unluckily, a greater number of women with OC go undiagnosed clinically till stages III and IV at which the 5-year survival rate is 20 to 25%.[1] So, early detection of OC is of utmost importance to decrease mortality due to this dreadful disease. Cancer Antigen-125 (CA-125) is a well-known biomarker in use and is generally proposed along with transvaginal ultrasound and clinical observations by clinical practice guidelines for the diagnosis of OC in adnexal mass patients.[2] But it has been stated that around 40 to 50% of women with early stage of the disease don’t exhibit deviated CA-125 levels.[3] Due to a lack of effective screening strategies to know the malignant potential of an adnexal mass, 7 out of 10 benign lesions were operated on. Some undergo substantial surgical staging comprising oophorectomy, increasing morbidity and risk of associated complications.[4] Moreover, in premenopausal women, the conservation of childbearing capacity is an important issue. So, accurate preoperative diagnostics comprising imaging techniques for differentiating masses is necessary for referring the correct patient to an expert gynecologic oncologist and to centers meant for proper management and care of OC patients that may improve the overall survival of the patients. The serum levels of biomarker CA-125 are often within the normal range at the onset of the disease and even in borderline tumors. Various benign conditions like endometriosis, fibroids, infections, pregnancy, menstrual phase, pelvic inflammatory disease, etc. influence the authenticity of results, as a false positive increase is seen in these conditions.[5,6] Ovarian masses are frequently found both in preand postmenopausal women. They can be benign or malignant. To study adnexal masses, transvaginal ultrasound is the first choice among imaging techniques that uses a power color Doppler to assess size, structure, and vascularization. According to previous data, approximately 8% of lesions comprising fibroids, struma ovarian tumors with low malignant potential and mucinous types, etc. stay undefined in sonography investigations of the adnexa. In such cases, noninvasive biomarker assessment may help in forming the diagnosis accurately.[7] Human Epididymis Protein 4 (HE4) is an upcoming biomarker in the differential detection of epithelial ovarian cancer (EOC) from benign masses and for monitoring response to chemotherapy. It was first detected in the epithelial lining of the distal epididymis. It was found to be a protease inhibitor that has a role in the maturation of sperm.[8,9] In its mature form, HE4 is a glycoprotein of 20 to 25 kDa present in the cytoplasm, the membrane of cells in the general circulation.[10,11] Its expression is also recognized in normal tissues like the glandular epithelium of the breast and female genital tract, distal epithelium of renal tubules, epithelium of the respiratory tract, salivary gland, etc.[12] Risk of malignancy Index (RMI) considers the menopausal status of patients, CA-125 serum levels, and transvaginal ultrasound findings. The combination of CA-125 and sonography of the pelvis in diagnosing women with OC may raise the sensitivity and specificity of the diagnosis.[13] Another anticipating model, called the Risk of Ovarian Malignancy Algorithm (ROMA) is used to approximate the risk of EOC in women having pelvic masses. It combines the values of HE4 and CA-125 in an algorithm based on menopausal status. ROMA may benefit in general practice where proficiency in gynecologic ultrasound is not available. It may help to sort women to an expert gynecologic center.[14] Hence, given this, we aim to evaluate the performance of biomarkers and algorithms in the detection of OC in women possessing suspected adnexal masses.
MATERIALS AND METHODS
Study Population
This case–control study was done at the Department of Biochemistry, Guru Gobind Singh Medical College and Hospital, Faridkot located in the cancer-prone Malwa belt of Punjab. The samples were collected from the Gynecology and Obstetrics Department of the same institution. We included 96 women 18 years of age or above diagnosed with an adnexal mass with suspected malignancy by ultrasound imaging and scheduled to undergo surgery by an expert gynecologist as patients for a period of 2 years. A total of 48 healthy females without any adnexal mass were taken as controls. We excluded women with pregnancy, previous history of cancer, chemotherapy, and concomitant diseases like chronic heart failure and renal disease or chronic liver disease. The permission of the Institutional Ethical Committee was taken vide letter no. GGS/IEC/18/83 to carry out the study. The samples were collected with the patient’s informed written consent.
Sample Collection and Analysis
A total of 5 mL of venous blood sample was withdrawn before surgery. Serum was collected after centrifugation and kept stored at —20°C until analysis. Women were further categorized into premenopausal (pre-M) and postmenopausal (post-M) groups. All women up to 50 years of age having menstruation within 1 year of the study sample collection were taken as pre-M, and women >55 years of age having no menses past 1 year of study sample collection were taken as post-M. For females above 40 and 50 years of age who had undefined last menstruation were confirmed by analyzing follicle-stimulating hormones (FSH). FSH levels > 30 mIU/mL or higher and having no menstruation for a year were considered confirmatory for postmenopause. CA-125 was analyzed by chemiluminescent immunoassay on a fully automated Access II analyzer (Beckman Coulter, Inc., United States). HE4 analysis was performed by the ELISA kit method (Calbiotech, Inc., EL Cajon, California, United States). ROMA combines serum HE4, CA -125, and menopausal status into a numerical score. ROMA is calculated as follows:
Before menopause: PI =− 12.0 + 2.38 × LN [HE4] + 0.0626 × LN [CA-125]
After menopause: PI =− 8.09 + 1.04 × LN [HE4] + 0.732 × LN [CA-125]
ROMA value (%) = ePI/[1 + ePI] × 100%. Here, PI indicates predictive index, LN indicates natural logarithm, e indicates base of the natural logarithm.[14]
RMI is a valuable clinical tool that combines CA-125, ultrasound findings, and menopausal status to calculate the risk of malignancy. The calculations were performed as suggested by Jacobs et al[13] as RMI = U × M × serum CA-125.
An RMI imaging score was calculated using the architectural features of the ovarian cyst or pelvic mass and was assigned with an imaging score as described by Jacobs et al.[13] Briefly, one point each was allocated to the following imaging findings, if present, as follows: multilocular cyst, solid nodule, bilateral cyst, ascites, and distant metastasis, where U = 0 for an ultrasound score of 0, U = 1 for an ultrasound score of 1, and U = 3 for an ultrasound score of 2 to 5 and M = 1 for pre-M women and M = 3 for post-M women.
To reduce biases in the study, patients with adnexal mass were selected randomly without knowing the malignant status of the mass and standard error was also calculated. After surgery, the masses were examined by an expert pathologist. Throughout the study, the results of the analysis were kept blinded from the pathologist’s view about the final pathology of the masses. At the end of the study, results were finally authenticated by reports of biopsy considering it as the gold standard. Patients with conditions that could affect biomarker levels like uterine fibroids, cancer, and menstruation were excluded. HE4 levels are known to be falsely raised in patients with renal diseases, so patients with renal diseases were also excluded from the study.
The cutoff for HE4 was taken as 70 and 140 pmol/L for preand post-M women, respectively. The cutoff for CA-125 was taken as 35 U/mL. The ROMA cutoffs for women at high risk as recommended by Moore et al[14] were taken as >13.1 and >27.7% for pre-and post-M women, respectively. The RMI cutoffs as put forth by Jacobs et al[13] were taken as 200 for distinguishing benign from malignant masses.
Statistical Analysis
The statistical analysis was done using SPSS 21. All study subjects were categorized based on menopausal status and final pathology of masses based on biopsy results into pre-and post-M and benign, malignant, and borderline masses groups, respectively. Comparisons were made between these by the Kruskal–Wallis test along with Tukey’s test. For all of the statistical comparisons, a level of p < 0.05 was accepted as statistically significant and standard error was also calculated. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated for CA-125, HE4, RMI, and ROMA. Receiver operating characteristic (ROC) curves were constructed, and the area under the curve (ROC-AUC) with a 95% confidence interval was calculated. Sensitivity and specificity were calculated in both pre-and post-M women separately. To identify patients with cancer, the best cutoff point of CA-125, HE4, and ROMA concerning best values of sensitivity, specificity, PPV, and NPV were also evaluated.
RESULTS
Our population under study included 96 women with adnexal masses anticipated to have surgery. The women were categorized based on menopausal status into preand post-M groups, respectively. The mean age of women in the pre-and post-M groups was 38 ± 8.2 and 58 ± 6.6 years, respectively.
Median levels of all the parameters were calculated in the study population based on the pathology of the masses. The levels of serum markers and predictive models comprising CA-125, HE4, ROMA, and RMI were compared between control, benign, borderline, and malignant groups. The sera levels of CA-125, HE4, and ROMA were significantly more in the benign group (p < 0.05) and malignant group (p < 0.001), compared with the control group. When we compared benign and malignant groups (p < 0.001), control and borderline groups (p < 0.05), all the markers have shown statistical significance; in contrast, benign and borderline groups (p > 0.05) were not significant. HE4, ROMA, and RMI (p < 0.05) were observed to be better markers in differentiating malignant from borderline tumors than CA-125 (p > 0.05) in our study (Table 1).
| Parameter | Controls N = 48 |
Benign N = 54 |
Malignant N = 36 |
Borderline N = 6 |
Total N = 96 |
|---|---|---|---|---|---|
| CA-125 (U/mL) | |||||
| Median | 15.6 | 17.4 | 259.8 | 70.1 | 45.8 |
| (Range) | (5.6–30) | (5.2–1057.2) | (11.7–5169) | (5.6–191) | (5.2–5169) |
| SE | 0.85 | 30.05 | 200.24 | 27.16 | 82.87 |
| HE4 (pmol/L) | |||||
| Median | 53 | 56.7 | 199 | 82.3 | 87.35 |
| (Range) | (26–66) | (25–159.2) | (70–938) | (49–131.7) | (25–938) |
| SE | 1.48 | 4.45 | 30.45 | 13.03 | 15.16 |
| ROMA (%) | |||||
| Median | 9.05 | 10 | 82.25 | 16.87 | 19 |
| (Range) | (2.8–15.8) | (1.5–74.1) | (25.9–98.9) | (7.4–42.2) | (1.5–98.9) |
| SE | 0.47 | 1.93 | 3.52 | 5.06 | 3.52 |
| RMI | |||||
| Median | – | 30 | 1414.5 | 199.3 | 118.8 |
| (Range) | (5.6–2406) | (105.3–16047) | (50.4–717) | (5.6–16047) | |
| SE | – | 58.07 | 873.88 | 111.91 | 373.92 |
CA-125, Cancer Antigen-125; HE4, Human Epididymis Protein 4; RMI, Risk of Malignancy Index; ROMA, Risk of Malignancy Algorithm; SE, standard error.
Note: p-Value of all markers (control/benign vs. malignant <0.001, control vs. benign/borderline <0.05, benign vs. borderline groups >0.05, malignant vs. borderline<0.05, except CA-125).
Table 2 depicted, most of the benign masses were found in the pre-M group (n = 37) versus (n = 17) in the post-M group, whereas malignant tumors were present mostly in the post-M group (n = 24) versus (n = 12) in the pre-M group. Among benign masses, the median and mean levels of CA-125 were more in the pre-M group supporting the fact that in pre-M women antigen levels can be raised because of conditions like endometriosis, adenomyosis, uterine fibroids, etc. Endometriosis was more commonly found in the pre-M group. CA-125 and RMI showed false high values (p < 0.001) but HE4 and ROMA did not rise significantly (p > 0.001) in endometriosis cases (n = 5) compared with rest of benign group.
| Parameter median (range) | Controls | Benign | Malignant | Borderline | ||||
|---|---|---|---|---|---|---|---|---|
| Pre- N = 25 |
Post- N = 23 |
Pre-M N = 37 |
Post-M N = 17 |
Pre-M N = 12 |
Post-M N = 24 |
Pre-M N = 4 |
Post-M N = 2 |
|
| CA-125 (U/mL) |
18.9 (10.2–26.5) |
13.2 (5.6–20.6) |
19.2 (5.2–1057.2) |
14.1 (5.1–802.9) |
226.7 (51.7–1382) |
294.8 (11.7–5169) |
66.45 (30–191) |
75.3 (5.6–145) |
| HE4 (pmol/L) |
45 (32–63) |
59 (26–66) |
57.8 (25–144) |
75 (26.7–159.2) |
221.5 (114–758) |
192.5 (70–938) |
70 (49–89.7) |
125.35 (119–131.7) |
| ROMA | 6.15 (3–10.4) |
9.8 (6–15.8) |
8.9 (1.5–56.3) |
12.75 (3–74.1) |
77.4 (38.2–98.6) |
83.45 (25.9–98.9) |
16.5 (7.4–27.5) |
28.5 (14.8–42.2) |
| RMI | – | – | 28.8 (5.6–1703.7) |
42.3 (15.6–2406) |
589.5 (155.1–4146) |
2173 (105.3–16047) |
199.3 (90–221.7) |
383.7 (50.4–717) |
CA-125, Cancer Antigen-125; HE4, Human Epididymis Protein 4; post-M, postmenopausal; pre-M, premenopausal; RMI, Risk of malignancy Index; ROMA, Risk of Malignancy Algorithm.
The sensitivity, specificity, PPV, and NPV were calculated considering borderline tumors in the malignant group. HE4 had lower sensitivity (87.5 and 78.5%) and NPV (93.9 and 80%) as compared with CA-125 (93.7 and 92.3%) and NPV (96.6 and 86.6%), in pre-and post-M women, respectively. In contrast, HE4 has improved specificity (83.7 and 94%) and PPV (70 and 95.6%) compared with CA-125 specificity (78.3 and 76.4%) and PPV (65.2 and 85.7%) in distinguishing benign pelvic mass from malignant masses in pre-and post-M women, respectively. This indicates that to enhance specificity we could contemplate HE4 estimations while making a differential diagnosis of an ovarian tumor. ROMA had similar sensitivity (93.7 and 92.3%) and almost the same NPV (96.2 and 88.8%) as CA-125 in pre-and post-M women, respectively, but showed improved specificity (94.1%) and PPV (96%) in post-M group. RMI showed lower sensitivity (68.7 and 88.4%) and NPV (86.5 and 83.3%) but higher specificity (86.4 and 88.2%) in pre-and post-M groups, respectively, compared with CA-125. Although RMI presented with the lowest sensitivity in the pre-M group, its specificity in this group is the highest (Table 3).
| Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | AUC | AUC overall | SE overall | p-Value | |
|---|---|---|---|---|---|---|---|---|
| CA-125 (35 U/mL) | 0.038 | <0.05 | ||||||
| Pre-M | 93.7 | 78.3 | 65.2 | 96.6 | 0.892 | 0.888 | ||
| Post-M | 92.3 | 76.4 | 85.7 | 86.6 | 0.907 | (0.813–0.963) | ||
| HE4 | 0.022 | <0.05 | ||||||
| Pre-M (70 pmol/L) | 87.5 | 83.7 | 70 | 93.9 | 0.926 | 0.947 | ||
| Post-M (140 pmol/L) | 78.5 | 94 | 95.6 | 80 | 0.955 | (0.904–0.989) | ||
| RMI≤200 | 0.024 | <0.05 | ||||||
| Pre-M | 68.7 | 86.4 | 68.7 | 86.5 | 0.916 | 0.937 | ||
| Post-M | 88.4 | 88.2 | 92 | 83.3 | 0.943 | (0.890–0.984) | ||
| ROMA PI | 0.021 | <0.05 | ||||||
| Pre-M≤13.1% | 93.7 | 70.2 | 57.6 | 96.2 | 0.927 | 0.949 | ||
| Post-M≤27.7% | 92.3 | 94.1 | 96 | 88.8 | 0.968 | (0.908–0.991) |
AUC, area under the curve; CA-125, Cancer Antigen-125; HE4, Human Epididymis Protein 4; NPV, negative predictive value; PPV, positive predictive value; post-M, postmenopausal; pre-M, premenopausal; RMI, Risk of malignancy Index; ROMA, Risk of Malignancy Algorithm; SE, standard error.
To define tumor biomarkers and screening tests, the ROC-AUC is often utilized since it delineates a convenient graphic tool for collating biomarkers and algorithms. It measures the differentiating ability of a test to distinguish between patients having the disease from those not having the disease. To find and compare the accuracy of diagnostic methods in pre-and post-M women for predicting malignant ovarian masses, ROC-AUC values were also measured.
We found that the ROMA in the overall, pre-M, and post-M groups with AUC (0.949, 0.927, 0.968) had maximum area associated with it followed by HE4 AUC (0.947, 0.926, 0.955). In the study population, overall ROMA performed better (AUC: 0.949) among all other markers (Table 3, Figure 1).
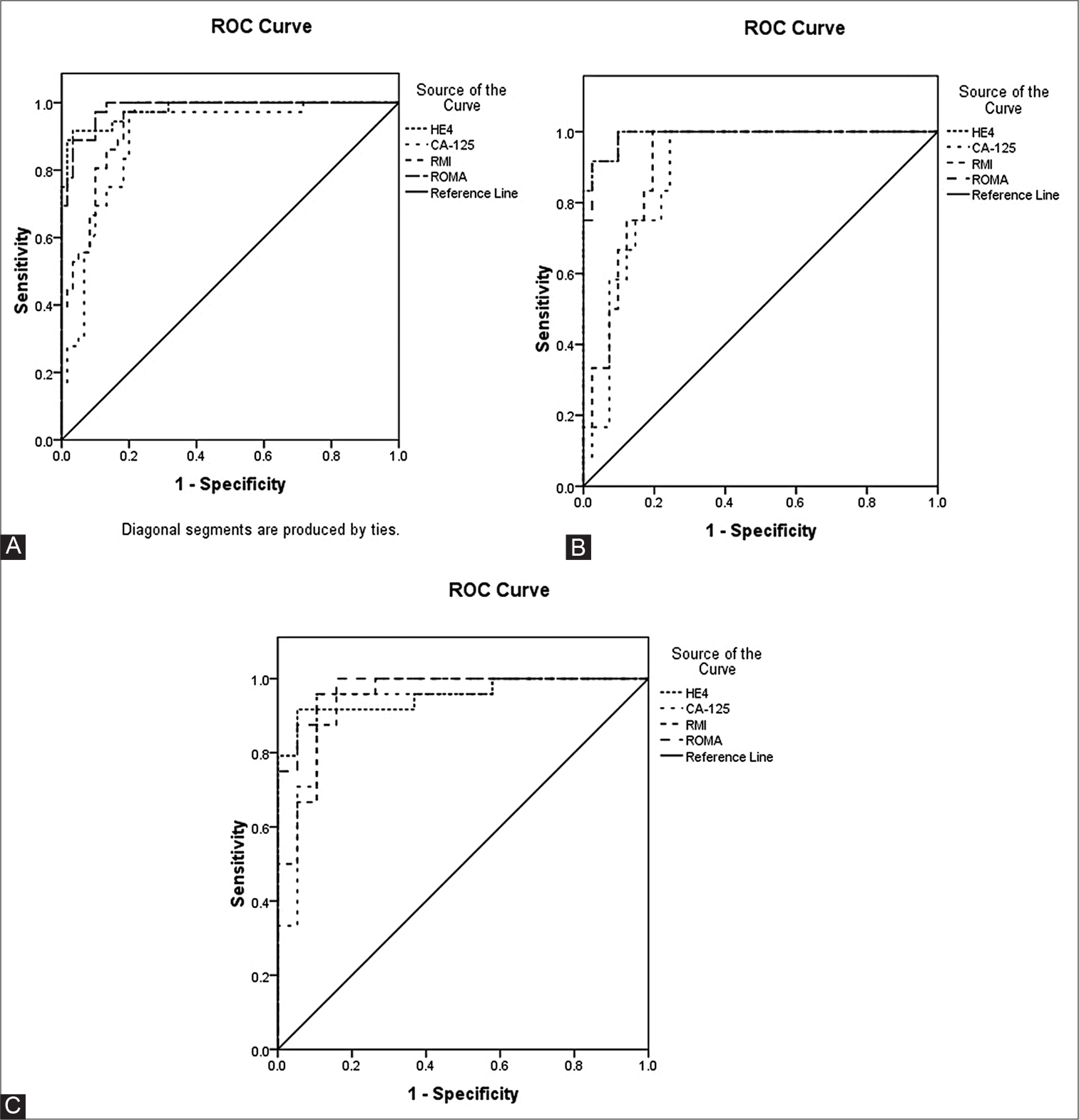
- Area under the receiver operating characteristic (ROC) curve of CA-125, HE4, ROMA, RMI. (A) Area under curve overall study population. (B) Area under the ROC curve premenopausal group. (C) Area under the ROC curve postmenopausal group. CA-125, Cancer Antigen-125; HE4, Human Epididymis Protein 4; ROMA, Risk of Malignancy Algorithm, RMI-Risk of malignancy Index.
In our study, ROC (AUC) curves were also calculated at best cutoffs obtained to find any improvement in sensitivity and specificity. The tumor marker CA-125, HE4, ROMA, and RMI displayed the best cutoff at 45.5, 47.25 U/mL; 72 and 130 pmol/L; 14 and 33.90; and 80.4 and 142 in preand post-M, respectively, at which great improvement in specificity of CA-125 (83.8 and 94.1%) is found in pre-and post-M groups. The sensitivity of HE4 (88.5%) and RMI (100 and 92.3%) increases in post-M and both groups, respectively. ROMA showed improvement in specificity to 78.4% in the pre-M group only (Table 4).
| Standard cutoffs |
Sensitivity (%) | Specificity (%) | Optimal cutoffs |
Sensitivity (%) | Specificity (%) | |
|---|---|---|---|---|---|---|
| ROMA (all) | 92.8 | 77.7 | 25.80% | 90.5 | 88.9 | |
| Pre-M | 13.1% | 93.7 | 70.2 | 14% | 93.8 | 78.4 |
| Post-M | 27.7%[14] | 92.3 | 94.1 | 33.90% | 92.3 | 94.1 |
| HE4 (all) | 85.7 | 87 | 130 | 81.0 | 96.3 | |
| Pre-M | 70 pmol/L | 87.5 | 83.7 | 72 pmol/L | 87.5 | 83.8 |
| Post-M | 140 pmol/L | 78.5 | 94 | 130 pmol/L | 88.5 | 94.1 |
| RMI (all) | 200[13] | 80.9 | 87 | 84.60 | 97.6 | 83.3 |
| Pre-M | 68.7 | 86.4 | 80.4 | 100 | 86.5 | |
| Post-M | 88.4 | 88.2 | 142 | 92.3 | 88.2 | |
| CA-125 (all) | 35 U/mL | 92.8 | 77.7 | 47.25 U/mL | 95.2 | 87.0 |
| Pre-M | 93.7 | 78.3 | 45.5 U/mL | 100 | 83.8 | |
| Post-M | 92.3 | 76.4 | 47.25 U/mL | 92.3 | 94.1 |
CA-125, Cancer Antigen-125; HE4, Human Epididymis Protein 4; post-M, postmenopausal; pre-M, premenopausal; RMI, Risk of Malignancy Index; ROMA, Risk of Malignancy Algorithm.
DISCUSSION
OC is a deadly gynecologic cancer because of its silent and symptomless nature of development. So, often diagnosed in the advanced stage leading to a poor prognosis. This was a case–control study examining the performance of serum biomarkers CA-125, HE4, and algorithms RMI and ROMA for the detection of OC in females with a suspected adnexal mass. Besides, we incorporated a normal population without adnexal mass in the control group of our study. We have consciously altered the above methods for the study using the available tools in general practice. For the ROMA, we used the CA-125 values done by chemiluminescent immunoassay on a fully automated Access II analyzer (Beckman Coulter, Inc., United States), because we generally perform the CA-125 test on the analyzer for our services and even though we wanted to make sure that the present study furnished a precise depiction of the tools available at our institution. We have used the same cutoff values suggested by Moore et al[14] and the RMI methods put forth by Jacobs et al.[13] RMI showed the highest specificity in our study as we have incorporated available computed tomography (CT) and magnetic resonance imaging (MRI) scans that could accurately define the features of masses besides ultrasound findings for calculating architectural features of masses. We are sure that the small variations made in the analysis shown here did not undermine the overall research findings of the study.
Our findings confirmed that among biomarkers, CA-125 had higher sensitivity (93.7 and 92.3%) than HE4 (87.5 and 78.5%), whereas HE4 had better specificity (83.7 and 94%) versus CA-125 (78.3 and 76.4%) in pre-and post-M groups, respectively. Our findings were further supported by a multicenter study by Lycke et al[15] with high sensitivity (96% pre-M, 92% post-M) and low specificity (60% pre-M, 80% post-M) of CA-125. In the same line, Anastasi et al[16] found a better sensitivity of CA-125 (90%) than HE4 (87%) and a lower specificity for CA-125 (70%) than HE4 (100%) in diagnosis EOC. Several meta-analyses support our findings.[17–19] HE4 second in line to ROMA displayed a higher AUC (0.947) than CA-125 (0.888). Richards et al[20] in a prospective study found better specificity of HE4 than CA-125 for the diagnosis of OC in all women as well as in pre-M women along with higher ROC-AUC for HE4 compared with CA-125 in all women. The AUC of CA-125 individually is weak. So, the use of CA-125 alone in diagnosis should be avoided strictly. The cutoffs of HE4 obtained in our study were in approximation to the recommended cutoffs of 70 and 140 pmol/L for pre-and post-M groups by Moore et al14 and are used in our study too.
ROMA had similar sensitivity (93.7 and 92.3%) and almost the same NPV (96.2 and 88.8%) as CA-125 in pre-and post-M groups, respectively, but showed improved specificity (94.1%) and PPV (96%) in post-M group. Compared with HE4 (sensitivity 85.7%, specificity 87%), ROMA has more sensitivity (92.8%) but less specificity (77.2%) overall. ROMA displayed the maximum AUC in the overall study population (AUC: 0.949), which was more than the AUC of CA-125 (0.88) and in approximation to the AUC of HE4 (0.947).
This was supported by the study of Chen et al[21] that found ROMA being more sensitive (96.7%) than HE4 (73.3%), but less specific (80 vs. 98.6%), respectively. The same study found no significant difference between AUC for ROMA and HE4 (0.97 and 0.96, respectively). Some recent studies support these results.[22,23] Terlikowska et al[24] also showed that ROMA (AUC: 0.918) compared with CA-125 and HE4 (AUCs: 0.895 and 0.879, respectively), performed better in differentiating EOC from benign ovarian disease. The cutoffs obtained for ROMA in our study are almost similar to the cutoff of 13.1% used by Moore et al[14] with not much difference in sensitivity and specificity.
RMI displayed better specificity (86.4%) in the pre-M group compared with CA-125 (78.3%). With an AUC of 0.916 in the pre-M group, it appears that the general performance of the RMI is good in pre-M, but because of a high false negative rate at the proposed cutoff of 200, a low sensitivity of only 68.6% in pre-M was found. RMI displayed better specificity compared with CA-125 as it is complemented by ultrasound/MRI/CT findings, but its low AUC does not make it the best diagnostic tool. The best cutoffs obtained for RMI in our study are different from the recommended cutoff of 200 pmol/L.
We reported that none of the markers under study was able to demarcate benign disease and borderline ovarian tumors significantly. However, a significant difference in levels of HE4, RMI, and ROMA excluding CA-125 was found when differentiating them from malignant disease. Endometriosis is a disease that often presents a diagnostic dilemma and interferes with diagnostic accuracy for evaluating the risk of malignancy. It often restricts the use of CA-125 as a marker to differentiate it from benign ovarian disease. The same was found in our study; CA-125 individually and RMI incorporating values of CA-125 were markedly falsely raised in endometriosis cases (n = 5) compared with benign cases. On the other hand, ROMA and HE4 were not falsely raised in endometriosis cases. We reported that in endometriosis, HE4 and ROMA measurements were better in performance than other methods. So, considering HE4 in the diagnosis of masses will complement CA-125. The raised specificity of HE4 for the distinction between endometriosis and OC is supported by recent studies[25,26] proposing that the use of CA-125 and HE4 together as in ROMA may improve differential diagnosis in this setting.
CONCLUSIONS
Despite small differences, the four methods under study (CA-125, HE4, RMI, and ROMA) were able to differentiate benign adnexal masses from malignant masses significantly and displayed similar levels of accuracy. The tumor markers HE4 and RMI displayed the best overall specificity for differentiating benign from malignant masses. CA-125 and ROMA displayed the best sensitivity. In our data, both HE4 and ROMA scores showed better performances with greater AUC. The incorporation of HE4 and ROMA will certainly improve diagnosis and will finally ameliorate the referral of patients to expert gynecologic centers, especially in settings where expert sonographers are not available. So, we suggest the use of ROMA and HE4 than a single traditional marker for differentiating masses. Although our study had certain limitations like the study population was small. Most of the malignant masses were in an advanced stage so we had to compare benign masses with advanced stage of malignancy, but still our results are worth noting.
Conflict of Interest
None declared.
Funding
None.
References
- Carcinoma of the ovary. Int J Gynaecol Obstet. 2006;95(Suppl 1):S161-S192.
- [CrossRef] [Google Scholar]
- Committee Opinion No. 477: the role of the obstetriciangynecologist in the early detection of epithelial ovarian cancer. Obstet Gynecol. 2011;117:742-746.
- [CrossRef] [PubMed] [Google Scholar]
- The HE4 (WFDC2) protein is a biomarker for ovarian carcinoma. Cancer Res. 2003;63:3695-3700.
- [Google Scholar]
- Long-term outcomes following conservative surgery for borderline tumor of the ovary: a large populationbased study. Gynecol Oncol. 2006;103:841-847.
- [CrossRef] [PubMed] [Google Scholar]
- Serum CA 125, carcinoembryonic antigen, and CA 19-9 as tumor markers in borderline ovarian tumors. Gynecol Oncol. 2000;78:16-20.
- [CrossRef] [PubMed] [Google Scholar]
- Benign causes of increased serum CA-125 concentration. Lancet Oncol. 2007;8:1054-1055.
- [CrossRef] [PubMed] [Google Scholar]
- Ovarian cancer biomarker performance in prostate, lung, colorectal, and ovarian cancer screening trial specimens. Cancer Prev Res (Phila). 2011;4:365-374.
- [CrossRef] [PubMed] [Google Scholar]
- Molecular characterization of epididymal proteins. Rev Reprod. 1998;3:86-95.
- [CrossRef] [PubMed] [Google Scholar]
- The evolution of a genetic locus encoding small serine proteinase inhibitors. Biochem Biophys Res Commun. 2005;333:383-389.
- [CrossRef] [PubMed] [Google Scholar]
- Monitoring gene expression profile changes in ovarian carcinomas using cDNA microarray. Gene. 1999;229:101-108.
- [CrossRef] [PubMed] [Google Scholar]
- The putative ovarian tumour marker gene HE4 (WFDC2), is expressed in normal tissues and undergoes complex alternative splicing to yield multiple protein isoforms. Oncogene. 2002;21:2768-2773.
- [CrossRef] [PubMed] [Google Scholar]
- Comprehensive analysis of HE4 expression in normal and malignant human tissues. Mod Pathol. 2006;19:847-853.
- [CrossRef] [PubMed] [Google Scholar]
- A risk of malignancy index incorporating CA 125, ultrasound and menopausal status for the accurate preoperative diagnosis of ovarian cancer. Br J Obstet Gynaecol. 1990;97:922-929.
- [CrossRef] [PubMed] [Google Scholar]
- A novel multiple marker bioassay utilizing HE4 and CA125 for the prediction of ovarian cancer in patients with a pelvic mass. Gynecol Oncol. 2009;112:40-46.
- [CrossRef] [PubMed] [Google Scholar]
- A multicenter clinical trial validating the performance of HE4, CA125, risk of ovarian malignancy algorithm and risk of malignancy index. Gynecol Oncol. 2018;151:159-165.
- [CrossRef] [PubMed] [Google Scholar]
- The use of HE4, CA125 and CA72-4 biomarkers for differential diagnosis between ovarian endometrioma and epithelial ovarian cancer. J Ovarian Res. 2013;6:44.
- [CrossRef] [PubMed] [Google Scholar]
- Human epididymis protein 4 for differential diagnosis between benign gynecologic disease and ovarian cancer: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2013;167:81-85.
- [CrossRef] [PubMed] [Google Scholar]
- Does risk for ovarian malignancy algorithm excel human epididymis protein 4 and CA125 in predicting epithelial ovarian cancer: a meta-analysis. BMC Cancer. 2012;12:258.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic accuracy of serum HE4, CA125 and ROMA in patients with ovarian cancer: a meta-analysis. Tumour Biol. 2014;35:6127-6138.
- [CrossRef] [PubMed] [Google Scholar]
- HE4, CA125, the Risk of Malignancy Algorithm and the Risk of Malignancy Index and complex pelvic masses a prospective comparison in the preoperative evaluation of pelvic masses in an Australian population. Aust N Z J Obstet Gynaecol. 2015;55:493-497.
- [CrossRef] [PubMed] [Google Scholar]
- Development of a multimarker assay for differential diagnosis of benign and malignant pelvic masses. Clin Chim Acta. 2015;440:57-63.
- [CrossRef] [PubMed] [Google Scholar]
- Distinguishing benign from malignant pelvic mass utilizing an algorithm with HE4, menopausal status, and ultrasound findings. J Gynecol Oncol. 2015;26:46-53.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of HE4, CA125 and ROMA algorithm in women with a pelvic mass: correlation with pathological outcome. Gynecol Oncol. 2013;128:233-238.
- [CrossRef] [PubMed] [Google Scholar]
- Preoperative HE4, CA125 and ROMA in the differential diagnosis of benign and malignant adnexal masses. J Ovarian Res. 2016;9:43.
- [CrossRef] [PubMed] [Google Scholar]
- Human epididymis protein 4 offers superior specificity in the differentiation of benign and malignant adnexal masses in premenopausal women. Am J Obstet Gynecol. 2011;205:e1-358.e6:358.
- [CrossRef] [PubMed] [Google Scholar]
- Serum HE4 concentration differentiates malignant ovarian tumours from ovarian endometriotic cysts. Br J Cancer. 2009;100:1315-1319.
- [CrossRef] [PubMed] [Google Scholar]






