Translate this page into:
Internal quality control of blood products: An experience from a tertiary care hospital blood bank from Southern Pakistan
Address for correspondence: Dr. Sadia Sultan, Department of Hematology and Blood Bank, Liaquat National Hospital and Medical College, Karachi, Pakistan. E-mail: sadiasultan96@yahoo.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
INTRODUCTION:
Internal quality control (IQC) is the backbone of quality assurance program. In blood banking, the quality control of blood products ensures the timely availability of a blood component of high quality with maximum efficacy and minimal risk to potential recipients. The main objective of this study is to analyze the IQC of blood products as an indicator of our blood bank performance.
METHODS:
An observational cross-sectional study was conducted at the blood bank of Liaquat National Hospital and Medical College, from January 2014 to December 2015. A total of 100 units of each blood components were arbitrarily chosen during the study. Packed red cell units were evaluated for hematocrit (HCT); random platelet concentrates were evaluated for pH, yield, and culture; fresh frozen plasma (FFP) and cryoprecipitate (CP) were evaluated for unit volume, factor VIII, and fibrinogen concentrations.
RESULTS:
A total of 400 units were tested for IQC. The mean HCT of packed red cells was 69.5 ± 7.24, and in 98% units, it met the standard (<80% of HCT). The mean platelet yield was 8.8 ± 3.40 × 109/L and pH was ≥6.2 in 98% bags; cultures were negative in 97% of units tested. Mean factor VIII and fibrinogen levels were found to be 84.24 ± 15.01 and 247.17 ± 49.69 for FFP, respectively. For CP, mean factor VIII and fibrinogen level were found to be 178.75 ± 86.30 and 420.7 ± 75.32, respectively.
CONCLUSION:
The IQC of blood products at our blood bank is in overall compliance and met recommended international standards. Implementation of standard operating procedures, accomplishment of standard guidelines, proper documentation with regular audit, and staff competencies can improve the quality performance of the transfusion services.
Keywords
Blood components
internal quality control
quality assurance
Introduction
Blood transfusion service (BTS) is the fundamental part of health-care system; deficiency causes impractical overall medical management. However, the blood transfusion is not free of risks owing to human factors; thus, it should only be prescribed when patients’ clinical statuses really necessitate it.[1] Transfusion services must have a standard obligation to endorse the optimal usage of blood components and to ensure that the final product causes minimal to zero risk to the potential recipient.
Internal quality control (IQC) is the backbone of the quality management program in the blood bank.[23] In the modern blood banking, quality controls of blood products ensure the timely availability of a blood component of high-quality yield with maximum efficacy and minimal risk to potential recipients.[4] Processes and manuals are need to be highly focused on generating quality blood components that are more efficacious and safe. The primary component in the quality control system is blood donation, which is collected from prospective donors of various ages with different demographics, health profiles, and risk behaviors. This blood collection process mainly depends on manual procedures which may have operator variations. Subsequently, these donations will be screened, stored, and transported under variant environmental circumstances.[5] These variants may compromise the critical control points which are designed to improve the quality of blood components.
In recent years, there have been significant developments aimed at improving the quality of the blood components. There have been advancement and progression in international standards for blood components, and principles of high-quality manufacturing practices have been redefined to provide the framework for quality in BTSs. This drive causes significant improvement in processes and blood component quality.
At national levels in Pakistan, BTSs are fragmented, semiautonomous, and asynchronized with nominal set criteria for quality assurance/control in transfusion services.[67] However, the effective implementation is yet questionable in most blood banks in the city. The purpose of this study is to determine the IQC on various blood products in a tertiary care center and to compare them with international set standard criteria.
Methods
Setting
A prospective cross-sectional study was conducted in the blood bank, Liaquat National Hospital and Medical College, from January 2014 to December 2015.
Material
In this period, 33,853 blood units were collected in sterile bags with an anticoagulant CPDA-1 (citrate phosphate dextrose adenine-1) having a volume of 63 ml, from healthy blood donors, who signed informed consent forms. Out of which, 100 units (a total of 400 units) of each blood components were arbitrarily chosen during the study, with the frequency of IQC testing once weekly for each product. All products were evaluated at the day of expiry (packed red blood cells [PRBCs] and platelets) or near expiry (fresh frozen plasma [FFP] and cryoprecipitate [CP]).
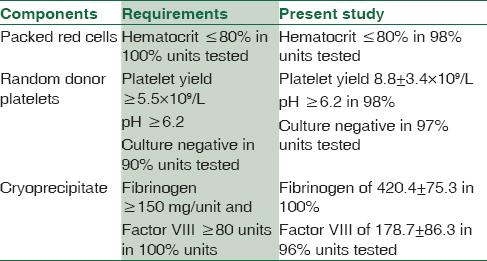
The American Association of Blood Banks (AABB) set standards for quality control assessment of blood component which was used for products evaluation as shown in Table 1.[8] Packed red cell units were evaluated for hematocrit (HCT) which was determined by CELL-DYN Ruby Hematology analyzer (Abbott, Diagnostic). Random platelet concentrates were evaluated for pH, yield, and culture; pH was detected by pH-indicator strips and universal indicator by Merck Millipore; yield was calculated by standard formula (platelets count × volume × 1000), and bacteriological culture analysis was achieved through the inoculation of samples in solid culture media (blood agar, chocolate, and MacConkey agar) and the brain-heart infusion medium. Culture plates were incubated at 37°C (±0.5) in Thermo Scientific incubator for 72 h. If no growth results was taken as negative, positive cultures further proceeded based on smear examination (Gram staining) and series of biochemical testing, which were performed to identify the bacterial species. FFP and CP were evaluated for unit volume, factor VIII, and fibrinogen concentrations; factor activities were evaluated by Sysmex® CA-1500-automated coagulation analyzer by clotting assay.
Ethical approval
The research protocol was approved by the Institutional Ethical and Research Committee, LNH, before the study.
Statistical analysis
Statistical Package for Social Sciences (SPSS) (Version 21.0, SPSS Inc, Chicago, IL, USA) for windows was used for analysis. The continuous data were described in terms of mean ± standard deviation while categorical data were depicted in frequencies.
Results
A total of 400 units were tested for IQC. The HCT of mean packed red cells was 69.5 ± 7.24 g/dl, and in 98% units (98 units out of 100), it met the standards with <80% of HCT. Remaining 2 units had HCT >80% with nonconformity to the norms.
Random donor platelets have shown the mean platelet yields of 8.87 ± 3.40 × 109/L and were in conformity with the norms in 94%, means only 6 (6%) units had yield <5.5 × 109/L; pH was ≥6.2 in 98% of units with the mean of 7.5 ± 0.8, and product cultures were negative in 97% of units tested. Three platelet units tested were positive for culture; species identification revealed Staphylococcus aureus in all units. To rule out bacterial contamination of whole blood, components (PRBCs and FFP) of positive units were tested, cultures were subsequently done, but found to be negative at all occasions. Virtually which rule out the possibility of bacterial contamination of units, invariably positive cultures were due to faulty sampling technique.
The mean factor VIII and fibrinogen levels were found to be 84.24 ± 15.01 and 247.17 ± 49.69 for FFP, respectively. Almost all donors have fibrinogen ≥150 mg/dl, while only five (5%) donors have factor VIII below the desired levels.
For CP, mean factor VIII and fibrinogen level were found to be 178.75 ± 86.30 and 420.7 ± 75.32, respectively. Among the 100 units tested, 100% were in conformity with the norms concerning the fibrinogen levels. The factor VIII assay was conformity with norms concerning their levels in 96%, while 4 (4%) units had levels below the recommendation.
Discussion
Blood banks have a dual liability primarily to meet the adequate blood supply for the community and essentially to ensure maximum blood recipient safety.[9] The safety and quality of blood components have been improved distinctly over the last two decades, owing to advancement in technology in all regions of the manufacturing processes, practices, and manuals. Processes are highly focused on producing high-quality products that are efficacious and are as safe as possible. Recently, the Food and Drug Administration commenced the concept of a “zero risk blood supply” as the manufacturing goal.[10]
Developing countries often face considerable obstacles to ensuring a safest blood transfusion. Recognizing quality control as a necessity, BTSs worldwide either have introduced or have been introducing. Quality management in transfusion services includes all requisites of blood supply chain including blood donation, appropriate blood collection, screening testing, component preparation, product storage, transportation, and secure transfusion to the recipients.
IQC is the central component of quality assurance program in transfusion services. IQC is the set of procedures undertaken for continuously and concurrently assessing blood bank work and the results, to decide whether the performance is up to the mark. IQCs play a vital role in blood transfusion safety, and risks allied with blood transfusion can be substantially reduced by the implementation of IQC.[11]
Pakistan is a developing country where BTSs are neither organized nor consistently regulated as they should be. The blood banks here are subjected to disorganized state, especially in respect to the quality controls, and they often do not always meet the necessary international standards. Keeping in mind these points, we formulated our present study to determine the IQC of blood products being prepared at our blood bank which is in a tertiary care center and compared the results with international set standard criteria. To date, a handful studies were reported from Asian countries in the literature on this aspect. To the best of our knowledge, this is the first report from our part of the world.
QC of blood products is the available tool to assess the viability of product, and consequently, it can adjust production techniques when necessary.[12] It is mandatory for all PRBCs, must have HCT of ≤80% (100%), as established by the AABB, but they do not recommend or set any lower acceptable limit.[8] However, it seems to be a useful decision to set appropriate range for HCT in the tested PRBCs. Raised PCV (2.0%) is the indirect indicator of faculty technique, which was seen in a small subset of units in the present study, which needs to be regularly evaluated, along with the technologist refresher training courses to retain and upgrade the manufacturing techniques.
Deliberated for more than 40 years, pH has been acknowledged as a decisive factor in ensuring platelets viability and has been used as a QC marker for the acceptability of platelets.[13] The FDA introduced platelet concentrates validation and minimum QC requirements in 1975.[13] Currently, FDA and AABB regulations require that QC testing of PLT components includes pH values of ≥6.2; culture should be negative, and platelets yield should be ≥5.5 × 109/l in 90% units tested.
We determined QC markers for platelets concentrate, which met the desired criteria in 97% of units. The mean pH of platelets was 7.5 ± 0.8, which is in consensus with other studies reported from the Western site. Previous studies from Canada and the United States have determined the mean pH of 7.3 ± 0.08 and meet the requirement in 98.1% of units tested, respectively.[1314] Fasola et al. from Nigeria reported that all (100%) the platelets concentrate preparations were within acceptable pH value of 7.25.[15]
We do not come across any study addressed the QC issues or evaluation of FFPs. The indications for transfusing FFP are limited in the current era due to the availability of recombinant or factor concentrates. FFP is generally not used in developed countries but developing countries like us largely depend on FFPs for various inherited coagulation defects. In view of its limited use, AABB do not recommend any standards for its testing. Our national standards and guidelines do recommend that FFPs have factor VIII >70 units in at least 75% of units.[16] Our findings were in conforms (95%) to local guidelines and standards.
The last but not the least is the IQC of cryoprecipitate, where quality control is regulated by factor assays. We determined the mean factor VIII and fibrinogen level to be 178.75 ± 86.30 and 420.7 ± 75.32, respectively. Surprisingly, among the 100 units tested, 100% were in conformity with the norms concerning the fibrinogen levels, rather mean value was quite high (420.7 ± 75.32) compared with the minimum (≥150 mg/unit) requirements. The factor VIII assay was conformity with norms concerning their levels in 96% of units, while four bags had levels below the recommendation, which requires corrective and preventive measures to be rectified in the near future.
Our present work is only a preliminary analysis; improved IQC in blood products and its methods need to be studied furthermore. Nevertheless, our research overlies the way for the establishment of a uniform national standard of IQC testing in Pakistan.
Conclusion
From the results, it can be concluded that the quality of blood components being prepared at our blood bank meets the international standards. Safe blood management is absolutely essential, and it is a universal human right which can be achieved by all national health-care systems through well-trained, motivated staff, quality kits, equipment's, facilities, efficient supervision, error and risk assessment system, good manufacturing practice guidelines, and adherence to standard operating procedures. Nevertheless, for all processes in blood collection, quality indicators should be defined, regularly monitored, documented, collated, evaluated, accounted, and consequently implemented.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank staff of the Blood Bank Division of Liaquat National Hospital and Medical College, for their excellent support.
References
- Serious Hazards of Transfusion (SHOT) haemovigilance and progress is improving transfusion safety. Br J Haematol. 2013;163:303-14.
- [Google Scholar]
- Performance assessment of internal quality control (IQC) products in blood transfusion compatibility testing in China. PLoS One. 2015;10:e0141145.
- [Google Scholar]
- Establishment and performance assessment of preparation technology of internal quality control products for blood transfusion compatibility testing. Exp Ther Med. 2013;5:1466-70.
- [Google Scholar]
- Quality of transfusion products in blood banking. Semin Thromb Hemost. 2014;40:227-31.
- [Google Scholar]
- Trends of venereal infections among healthy blood donors at Karachi. Arch Iran Med. 2016;19:192-6.
- [Google Scholar]
- Components from whole blood donations. Technical Manual, American Association of Blood Banking (AABB) 2005:202.
- Adverse reactions in allogeneic blood donors: A tertiary care experience from a developing country. Oman Med J. 2016;31:124-8.
- [Google Scholar]
- The quest for quality blood banking program in the new millennium the American way. Int J Hematol. 2002;76(Suppl 2):258-62.
- [Google Scholar]
- Participation in proficiency programs and promotion of quality in transfusion services of Minas Gerais. Rev Bras Hematol Hemoter. 2012;34:21-4.
- [Google Scholar]
- Platelet aggregation and quality control of platelet concentrates produced in the amazon blood bank. Rev Bras Hematol Hemoter. 2011;33:110-4.
- [Google Scholar]
- The value of pH as a quality control indicator for apheresis platelets. Transfusion. 2005;45:773-8.
- [Google Scholar]
- Development of a quality monitoring program for platelet components: A report of the first four years’ experience at Canadian Blood Services. Transfusion. 2012;52:810-8.
- [Google Scholar]
- Quality assessment of platelet concentrate prepared at a tertiary centre in Nigeria. Afr J Med Med Sci. 2002;31:337-9.
- [Google Scholar]
- Standards and Guidelines for Blood Banks and Transfusion. Safe Blood Transfusion Programm- SBTP (1st). Islamabad: Government of Pakistan; 2013. p. :22-3.





