Translate this page into:
Malignant melanoma of conjunctiva: Diagnosis on fine-needle aspiration cytology
Address for correspondence: Dr. Vijay Kumar, Department of Pathology, Room No 314, 3rd Floor, OPD Building, Dr. Ram Manohar Lohia Hospital, Baba Kharak Singh Maarg, New Delhi - 110 001, India. E-mail: vijaypgi1@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Malignant melanoma of conjunctiva is an uncommon malignancy. The diagnosis is suspected clinically and confirmed on pathological examination. We present a case of a 63-year-old female with previous history of pigmented lesion in the right eye and subsequently diagnosed as malignant melanoma of right conjunctiva and cornea on fine-needle aspiration cytology and histopathology.
Keywords
Conjunctiva
cornea
fine-needle aspiration cytology
melanoma
Introduction
Malignant melanoma of the conjunctiva arises from the malignant proliferation of melanocytes. It can arise de novo or from a preexisting nevus or primary acquired melanosis (PAM).[123] Routine surgical biopsy of globe and deeply seated orbital lesions need aggressive procedures: anesthesia; and operating room. In comparison, fine-needle aspiration cytology (FNAC) is minimally invasive and much cheaper with fast results.[3456] We report a case of malignant melanoma of conjunctiva (right eye) on FNAC and confirmed on histopathology with encroachment over cornea.
Case Report
A 63-year-old female presented with pigmented and elevated lesion measuring approximately 0.8 cm × 0.8 cm, in the right eye for the last 1.5–2 years [Figure 1a]. Initially, the lesion had started as a thin black thread-like area; however, rapid increase in the size of lesion was noted in the past 1 month. Ocular examination revealed presence of cataract in both eyes with hazy corneal opacities. There was no difficulty in reading or vision. No blackish discoloration or such lesions were noted elsewhere in the body.
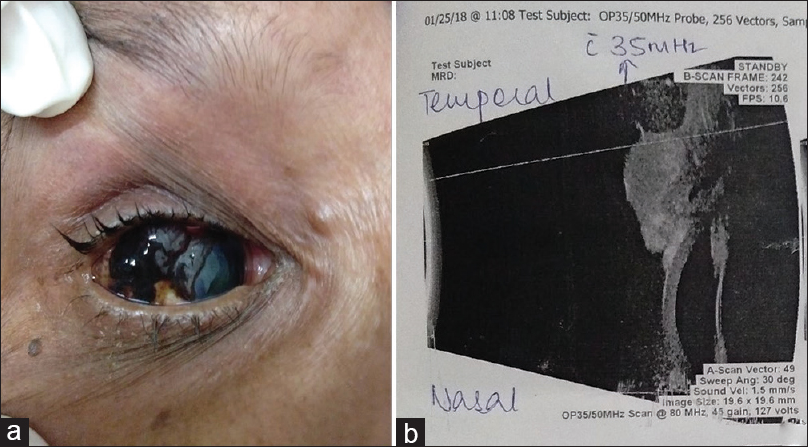
- (a and b) A pigmented and elevated lesion measuring approximately 0.8 cm × 0.8 cm, in the right eye encroaching over conjunctiva and cornea along with hazy corneal opacity, suggestive of cataract. (b) B-mode ultrasound revealed an eyelid and conjunctival lesion (? melanoma) with encroachment on cornea of the right eye
Her complete blood counts and biochemical parameters including liver and kidney function tests, serum electrolytes, blood sugar, and thyroid profile were within normal limits. B-mode ultrasound was done and a provisional diagnosis of a conjunctival lesion (? melanoma) with encroachment on cornea of the right eye [Figure 1b]. Her left eye showed evidence of macular hole.
Fine-needle aspiration (FNA) was done with extreme precaution under guidance of ophthalmologist. Eyeball was fixed using the ocular speculum, following which 22-gauze needle was inserted and minimal aspiration was done. Then, immediately gauze piece was put over the eye to give pressure and avoid any bleeding. FNA smears from the blackish lesion over right conjunctiva were highly cellular and comprised predominantly singly scattered tumor cells along with few groups and clusters [Figure 2a and b]. Tumor cells showed moderate pleomorphism and were round to oval to spindle-shaped with central to eccentrically placed nuclei, coarse chromatin, prominent inclusion-like nucleoli, and moderate amount of cytoplasm [Figure 2c and d]. Intracellular and extracellular blackish-brown pigment (melanin) was seen at places [Figure 2a-d]. Many binucleated, multinucleated, and bizzare forms were also noted [Figure 2a-d].
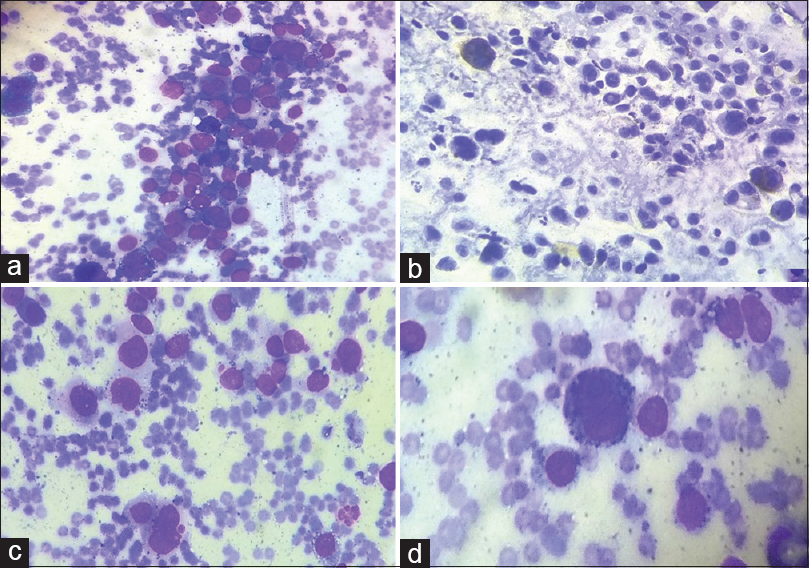
- (a-d) Fine-needle aspiration smears from the ocular lesion revealing high cellularity and composed of predominantly singly scattered tumor cells along with few groups and clusters showing moderate pleomorphism (a and b) with round to oval to spindled-shaped cells with central to eccentrically placed nuclei, coarse chromatin, prominent inclusion-like nucleoli (d) and moderate amount of cytoplasm. Many binucleated, multinucleated, and bizarre forms (a-d) are noted along with intracellular and extracellular blackish brown pigment (melanin) (a: Giemsa, ×200; b: Pap, ×200, c: Giemsa, ×400, d: Giemsa, ×1000)
Positron-emission tomography-computed tomography scan showed mildly fluorodeoxyglucose (FDG) avid enhancing soft-tissue thickening involving the right anterolateral aspect of right globe, representing a primary mitotic lesion. No evidence of FDG avid visible mitotic disease was noted elsewhere in the body.
Based on the clinicoradiological and cytopathological evaluation, a diagnosis of “Malignant Melanoma” was given. The patient was referred to a higher center for further surgical management. A wide local excision was done with lamellar dissection of cornea. Excised conjunctival mass showed features compatible with malignant melanoma (epithelioid cell type with ulceration of overlying conjunctiva) [Figure 3a]. The tumor cells showed positivity for Melan-A [Figure 3b] and S100 [Figure 3c], thereby confirming the diagnosis of malignant melanoma. The excised margin showed evidence of PAM with atypia. The separately sent lid margin also showed evidence of malignant melanoma along with features of PAM and atypia. A final diagnosis of malignant melanoma of conjunctiva with extension into the cornea as well as eyelid, including canthus (ICD-C43.1), was made. Postoperatively, the patient was given antibiotics (Tablet Augmentin) for 5 days along with lubricant eye drops and is currently under follow-up.
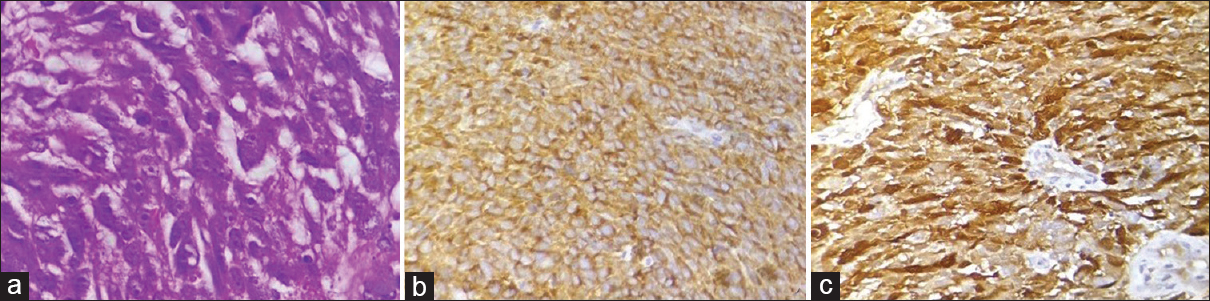
- (a-c) Section showing a highly cellular tumor composed of epithelioid cells with high N/C ratio, prominent eosinophilic nucleoli (H and E, ×400); (b and c) tumor cells showing positivity for Melan A (b, ×400) and S100 (c, ×400)
Discussion
Melanoma is an aggressive tumor of the melanocytes. Primary melanomas usually involve the skin, mucosa, retina, and leptomeninges.[234] However, melanomas can metastasize to lymph nodes, lung, and liver.[5] Cytopathology has a key role in distinguishing pigmented lesions of the eye which can be benign, premalignant, or frankly malignant lesions.[23456]
The different approaches for doing orbital FNA include transscleral, transcorneal, or transvitreal, using 25–30-gauge needle.[234] Nonaspiration technique is preferable for tiny and vascular lesions. In case of suspected conjunctival melanoma, imprint cytology (IC) using cellulose acetate strips has been found to be very useful. Gross nature of the cytologic material in cases of pigmented melanoma is usually blackish and fluid-like as noted in our case.
Various cytologic techniques used in the diagnosis of ocular lesions are FNAC, IC, and scrape cytology. Although the most commonly used cytologic technique is the FNA, exfoliative and IC are also used depending on the size and location of the lesion.[5678] Although diagnostic biopsy remains necessary for the determination of the origin and extent of the lesions, the use of cytology can minimize the frequency of biopsy in selected cases.
Fine-needle smears from melanocytic lesions show high cellularity composed of a predominant population of dissociated cells with nuclear pleomorphism, plasmacytoid, with eccentrically placed nuclei, polygonal or spindle cells; macronucleoli; intra-nuclear cytoplasmic inclusions; increased mitotic activity; and variable number of bi- and multinucleated cells. Melanotic melanomas show a variable amount of intra- and extra-cellular pigment. The index case also showed extracellular and intracellular pigment. Even the cases of amelanotic melanomas often exhibit coarse or fine-pigment granules in rare or, a few cells which can be picked up on careful cytologic examination.
The cytologic diagnosis of amelanotic melanoma is difficult because in the absence of pigment, the tumor cells may mimic those of carcinoma or sarcoma in cytologic samples, particularly those obtained by FNA. Irregular nuclear outline and coarse chromatin are the features common to any of the malignant lesions, which are also applicable for melanoma cells. Of the general cytomorphologic features elaborated above, intranuclear cytoplasmic inclusions are of diagnostic importance, only in conjunction with other cytomorphologic and clinical features. Various disease entities such as papillary thyroid cancer, medullary thyroid cancer and anaplastic thyroid carcinomas; bronchioloalveolar carcinoma, hepatocellular carcinoma, and renal cell carcinoma show intranuclear and cytoplasmic inclusion but can be easily differentiated with the help of clinic-radiological details.
In our case also, the patient had a pigmented lesion, PAM; however, the initial diagnosis was not made, and patient presented to us with increased blackish mass in the right eye encroaching over the conjunctiva and cornea. Conjunctival melanomas are potentially lethal, and they arise in association with preexisting PAM.[234] Our patient also presented with similar findings with a history of PAM a year ago, and currently on admission, she had an increased blackish mass in the right eye. It is important to recognize and monitor precursor lesion owing to its malignant potential. It has been noted in few studies that malignant melanoma of eyelid with involvement of cornea and conjunctiva has poorer prognosis.[91011] Follow-up of suspicious conjunctival lesions by repeated biopsies may cause symblepharon, lid deformities, and discomfort to the patient.
The use of ancillary aids such as immunocytochemistry and electron microscopy is of critical value in the diagnostically challenging cases. Various immunohistohistochemical stains helpful in making diagnosis are S100, Melan-A, and HMB-45. Other differential diagnosis which should be kept in mind while evaluating these lesions are nevus, basal cell carcinoma, sebaceous gland carcinoma, Merkel cell tumor, or any metastasis. Hence, a detailed cytological and histological finding along with clinical correlation is important to differentiate these lesions.
Surgical excision along with adequate margins is the treatment of choice for melanoma.[891011] The prognosis of melanoma varies with the site and stage of the disease. Advanced disease with local recurrence or distant metastasis carries a grave prognosis.
Conclusion
Malignant melanoma of conjunctiva is a rare disease entity. The involvement of conjunctiva and cornea makes the prognosis poor. Hence, an early diagnosis of malignant melanoma is important to decrease the extent of disease and preventing any further complications in the patient. Although histopathology remains the gold standard in the definitive diagnosis of malignant melanoma, a simple investigative modality, that is, FNAC in conjunction with clinicoradiological findings can help in making an early diagnosis in the patient.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Transscleral fine-needle aspiration biopsy of macular choroidal melanoma. Am J Ophthalmol. 2008;145:297-302.
- [Google Scholar]
- Malignancy in the blind painful eye – Report of two cases and literature review. Diagn Pathol. 2006;1:45.
- [Google Scholar]
- The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma, III: Initial mortality findings. COMS report no 18. Arch Ophthalmol. 2001;119:969-82.
- [Google Scholar]
- Iris melanoma: Risk factors for metastasis in 169 consecutive patients. Ophthalmology. 2001;108:172-8.
- [Google Scholar]
- Uveal melanoma: Epidemiologic aspects. Ophthalmol Clin North Am. 2005;18:75-84, viii.
- [Google Scholar]
- Fine needle capillary sampling of eyelid masses. A study of 70 cases. Acta Cytol. 2003;47:349-58.
- [Google Scholar]
- Benign skin adenexal tumor vs.hemangioma: Diagnostic pitfall due to cytologic sampling error. Acta Cytol. 2008;52:378-80.
- [Google Scholar]
- Fine needle aspiration biopsy in pigmented basal cell carcinoma. Acta Cytol. 2008;52:509-11.
- [Google Scholar]
- Cytomorphologic features of sebaceous carcinoma on fine needle aspiration. Acta Cytol. 2000;44:760-4.
- [Google Scholar]





