Translate this page into:
Platelet and erythrocyte parameters in type 2 diabetic moroccan patients: A cross-sectional study
*Corresponding author: Ibtissam Mhirig, MD, Department of Biochemistry, Mohammed VI University Hospital, Marrakech, 40000, Morocco ibtissam96mhirig@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mhirig I, Harrar S, Habibi L, Sayagh S, Aboulmakarim S. Platelet and erythrocyte parameters in type 2 diabetic moroccan patients: A cross-sectional study. J Lab Physicians. 2024;16:52-7. doi: 10.1055/s-0043-1774811
Abstract
Objectives:
Complete blood count parameters have gained renewed interest as predictors of endothelial dysfunction in type 2 diabetes mellitus (T2DM). Thus, the aim of this study was to observe the changes in platelet and erythrocyte parameters between diabetics and nondiabetics and to evaluate these changes in relation to glycemic control.
Materials and Methods:
This cross-sectional study was performed in Mohammed VI University Hospital, Marrakech, Morocco, from January 2020 to July 2021. A total of 307 Moroccan patients were enrolled in this study, which included 222 diabetic patients and 85 nondiabetics. The diabetic patients were divided into two groups A (hemoglobin A1c [HbA1c] ≤ 6.5%) and B (HbA1c < 6.5%) according to their glycated hemoglobin levels (HbA1c). Biological parameters were processed as per the standard technique. Data analysis was performed using SPSS statistical software.
Statistical Analysis:
Data were analyzed using SPSS 23 software (Statistical Package for Scientific Studies; IBM Corp. Armonk, New York, United States), and it was described as mean and standard deviation.
Results:
A significant difference was mentioned regarding mean corpuscular volume (MCV) (p < 0.001), red blood cell distribution width (RDW) (p < 0.001), and volume/platelet count (p = 0.023) between diabetics and nondiabetics. MCV and RDW were lower in group B than group A (p = 0.004; p = 0.04), while MPV was higher (p = 0.342). RDW significantly and negatively correlated with HbA1c in diabetic population (r = –0.182; p = 0.006). On the other hand, a significant and positive correlation between MPV and HbA1c was mentioned (r = +0.184; p = 0.006).
Conclusion:
Our study showed that RDW and MPV correlate with HbA1c in T2DM and can be used as a reproducible and inexpensive means to ensure proper control of glycemic status. Further studies are warranted to define specific RDW and MPV values predictive of complication risk in the diabetic population.
Keywords
glycated hemoglobin
mean platelet volume
red cell distribution width
type 2 diabetes mellitus
INTRODUCTION
Type 2 diabetes mellitus (T2DM) is a global health problem due to its high morbidity.[1] Management, regular follow-up with assessment of complications, and monitoring of blood glucose levels still remain a great challenge for any health care provider, especially in low socioeconomic countries. In this regard, glycated hemoglobin (HbA1c) is used as a tool for glycemic control, and since 2010, it is also accepted for the diagnosis of diabetes. It is an index of glycemic control over a period of 8 to 12 weeks.[2]
Hematological changes in diabetes mellitus can be caused by several factors, including increased production of reactive oxygen species that lead to oxidative stress involved in tissue damage and hematological functional and structural changes, such as dysfunction of the hemoglobin molecule, the cytoplasmic environment of individual red blood cells, hyperactivity of blood platelets, and endothelial dysfunction.[3,4] Hematological parameters, such as red blood cell distribution width (RDW), mean platelet volume (MPV), platelet distribution width (PDW), and platelet count, have gained renewed interest as predictors of endothelial dysfunction in T2DM.[5,6] Numerous studies have shown that platelet and erythrocyte indices show an increasing or decreasing trend in diabetic patients, which is not the case in nondiabetic patients.[7,8]
Thus, the aim of this current study was to observe the changes in platelet and erythrocyte parameters in diabetic patients compared with nondiabetic ones, and to evaluate these changes in relation to glycemic control, based on biological parameters derived from complete blood count which is a simple, inexpensive, and commonly used technique in practice.
MATERIAL AND METHODS
This cross-sectional study was conducted in the biochemistry laboratory of Mohammed VI University Hospital, Marrakech, Morocco, from January 2020 to July 2021 having enrolled a total of 307 patients, 222 T2DM patients and 85 control patients.
Diabetes mellitus was defined according to the American Diabetes Association criteria: HbA1c ≥ 6.5% or fasting blood glucose (FBG) ≥ 126 mg/dL or 2-hour blood glucose ≥ 200 mg/dL on an oral glucose tolerance test.
The study protocol was approved by the Ethics Committee of University Hospital of Marrakech (N° 43/2023/9 Mai, 2023). All subjects underwent relevant routine laboratory testing of venous blood samples collected in ethylenediaminetetraacetic acid tripotassium or dry tube based on type of the assay.
We excluded patients with other main types of diabetes mellitus than T2DM, a history of hemoglobinopathies, other causes of anemia, chronic diseases (chronic liver disease, chronic renal failure, and chronic inflammatory rheumatism), acute and chronic infections, malignant tumors, thrombocytopenia, or thrombocytosis.
XT-4000i (Sysmex, Japan) hematology analyzer was used to measure blood parameters. HbA1c was analyzed by the G8 HPLC Analyzer (Tosoh, Griesheim, Germany), while FBG was analyzed by Cobas 6000 analyzer (Roche, Basel, Switzerland).
Calibration, quality control, and sample processing were performed according to the manufacturer’s instructions.
Diabetics were divided into two groups: group A = good glycemic control (HbA1c < 6.5%) and group B = poor glycemic control (≥ 6.5%). The groups were compared according to platelet parameters: MPV, platelet count, PDW, and volume/platelet count, and red blood cell parameters: RDW, hemoglobin, and mean corpuscular volume (MCV).
Data were analyzed using SPSS 23 software (Statistical Package for Scientific Studies; IBM Corp. Armonk, New York, United States), and it was described as mean and standard deviation.
Normality of the parameters was examined using KolmogorovSmirnov tests, and homogeneity of variances was checked by the Leven’s test. Comparison of the means of the hematological parameters between diabetic patients and controls was performed by the independent t-test for normally distributed data with homoscedasticity of variances, and the Mann– Whitney U test for data with a nonnormal distribution or with noncomparable variances. Correlation between the different variables was performed using the Pearson’s momentary correlation equation for normally distributed data, and RhoSpearman for variables with a nonnormal distribution.
A p-value of ≤ 0.05 was considered statistically significant.
RESULTS
Of the 307 patients that were found eligible for the study, 62.3% were women and 37.7% were men.
Patients were divided into two groups: Diabetic group (n = 222) and control group (n = 85). The mean age of diabetic patients in our study was 61.90 ± 9 years and that of the control group was 53.19 ± 13 years.
Platelet and erythrocyte indices have been compared between both groups. The results showed a statistically significant difference regarding MCV (p < 0.001), RDW (p < 0.001), and volume/platelet count (p = 0.023). There was no difference in hemoglobin and in other platelet parameters (MPV, PDW, and platelet count) as shown in Table 1.
| Parameters | Diabetic group (n = 222) | Control group (n = 85) | p-Value |
|---|---|---|---|
| Age | 61.90 ± 9 | 53.19 ± 13 | < 0.001* |
| HbA1c | 8.1 ± 1.63 | 5.66 ± 0.43 | < 0.001* |
| FBG | 1.62 ± 0.72 | 0.91 ± 0.13 | < 0.001* |
| Hemoglobin | 13.61 ± 1.27 | 13.51 ± 1.34 | 0.568 |
| MCV | 86.21 ± 6.07 | 99.04 ± 84.30 | < 0.001* |
| RDW | 42.7 ± 3.8 | 46.35 ± 6.45 | < 0.001* |
| Platelet count | 270.42 ± 97.09 | 257.70 ± 77.12 | 0.503 |
| MPV | 11.48 ± 4.53 | 11.32 ± 1.07 | 0.631 |
| PDW | 0.60 ± 0.11 | 0.56 ± 0.10 | 0.106 |
| Volume/platelet count | 34.50 ± 11.6 | 30.12 ± 14.04 | 0.023* |
FBG, fast blood glucose; HbA1c, glycated hemoglobin; MCV, mean corpuscular volume; MPV, mean platelet Volume; PDW, platelet distribution width; RDW, red distribution width; SD, standard deviation.
mstatistically significant result.
We also categorized the diabetic patients into two groups according to the HbA1c levels: group A containing 23 patients with good glycemic control (HbA1c < 6.5%), and group B including 199 patients with a poor glycemic control (HbA1c ≤ 6.5%) (Table 2).
| Parameters | Diabetic population group A Hba1c<6.5 (n = 23) | Diabetic population group B Hba1c≤6.5 (n = 199) | p-Value |
|---|---|---|---|
| Age | 62.21 ± 9.25 | 59.22 ± 8.52 | 0.141 |
| HbA1c | 8.35 ± 1.55 | 6.02 ± 0.38 | < 0.001* |
| FBG | 1.65 ± 0.72 | 1.34 ± 0.70 | 0.005 |
| Hemoglobin | 13.71 ± 1.39 | 13.6 ± 1.26 | 0.672 |
| MCV | 89.40 ± 4.81 | 58.85 ± 6.10 | 0.004* |
| RDW | 44.50 ± 5.19 | 42.48 ± 3.55 | 0.04* |
| Platelet count | 267.80 ± 91.85 | 293.21 ± 134.77 | 0.50 |
| MPV | 11.12 ± 1.02 | 11.35 ± 1.08 | 0.342 |
| PDW | 0.60 ± 0.11 | 0.56 ± 0.10 | 0.148 |
| Volume/platelet count | 34.62 ± 11.71 | 33.37 ± 11.60 | 0.253 |
FBG, fast blood glucose; HbA1c, glycated hemoglobin; MCV, mean corpuscular volume; MPV, mean platelet volume; PDW, platelet distribution width; RDW, red distribution width.
mstatistically significant result.
The mean MCV in group B (58.85 ± 6.1023) was significantly lower than in group A (89.40 ± 4.81; p = 0.004). The mean RDW level in group A was 44.50 ± 5.19 while that of group B was 2.48 ± 3.55 (p = 0.04). The MPV in group B (11.12 ± 1.02) was higher than in group A (11.35 ± 1.08) but was not statistically significant (p = 0.342). No significant correlation was identified for PDW (p = 0.34), platelet count (p = 0.50), and volume/platelet count (p = 0.25).
Moreover, we studied correlations between HbA1-c/fasting plasma glucose and MPV/RDW in diabetic patients. Table 3 and Figure 1 show clearly a statistically significant positive correlation between MPV and HbA1c (p = 0.006, r = 0.184), whereas MPV was not correlated with FBG (p = 0.092, r = 0.198). RDW was inversely associated with FBG (r =–0.122; p = 0.084) and HbA1c (r =–0.182; p = 0.006) as shown in Table 3 and Figure 2.
| Parameters | r-Value | p-Value | |
|---|---|---|---|
| MPV | HBA1c | 0.184 | 0.006 |
| MPV | FBG | 0.198 | 0.092 |
| RDW | Hba1c | –0.182 | 0.006 |
| RDW | FBG | –0.122 | 0.084 |
FBG, fast blood glucose; FPG, fasting plasma glucose; HbA1c, glycated hemoglobin; MPV, mean platelet Volume; RDW, red distribution width.
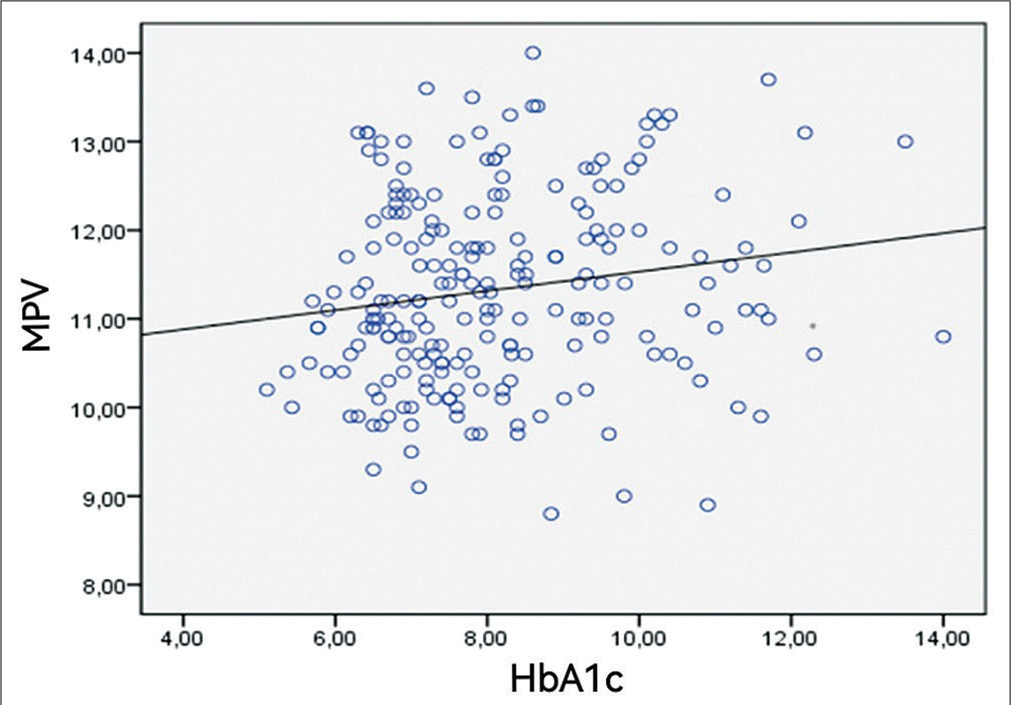
- Pearson’s correlation showing a linear relation between mean platelet volume (MPV) and hemoglobin A1c (HbA1c) in diabetics.
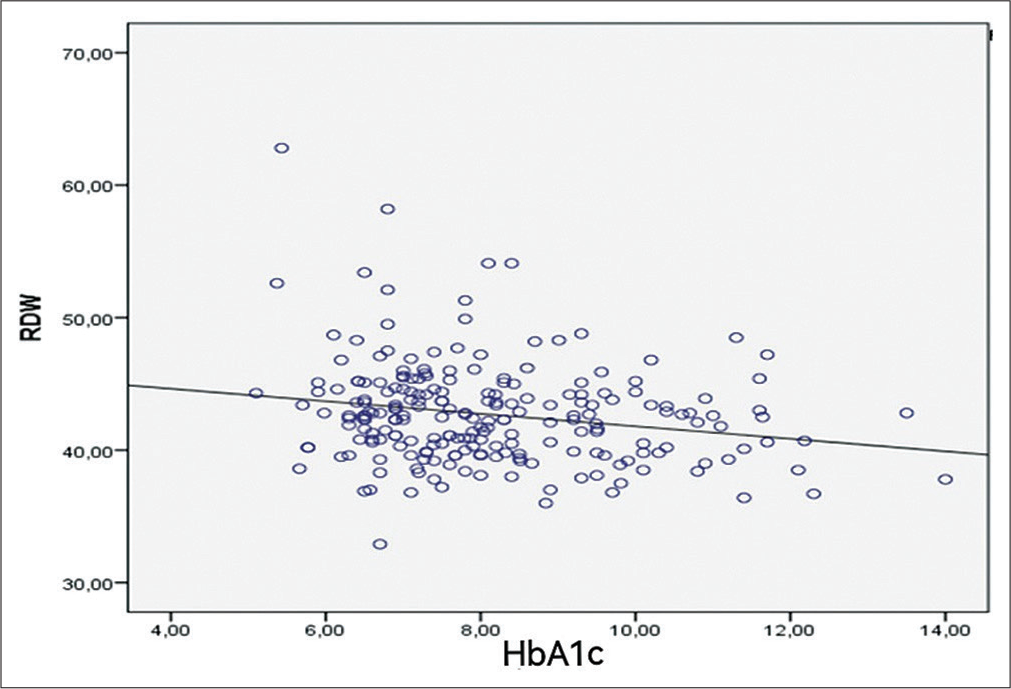
- Pearson’s correlation showing a linear relation between red blood cell distribution width (RDW) and hemoglobin A1c (HbA1c) in diabetics.
DISCUSSION
Hematologic changes are a common complication of diabetes and represent a significant and unrecognized burden in these patients.[9] Slow glycosylation and constant elevation of HbA1c may be associated with functional and structural changes in the hemoglobin molecule, and in the cytoplasmic viscosity of individual red cells, and may affect any or all of the red cell parameters.
RDW is one of the red cell parameters whose values are easily calculated in a blood count, thus constituting a simple and inexpensive routine examination.[10] Although it assesses the variability of red blood cell size within the bloodstream,[11,12] it is recently considered to be a marker of inflammation in the incidence of atrial fibrillation and heart failure with significant predictive value for mortality in healthy and sick patients.[13,14]
A recent study by Tsilingiris et al involving 183 patients, 83 with T2DM and 100 nondiabetic patients, showed a positive correlation between HbA1c and RDW in nondiabetics (p = 0.001; r = 0.315), and negative in diabetics (p = 0.011; r =–0.275).[15] Indeed, in nondiabetics, RDW acts as an index of biological interference on HbA1c measurement, caused by both normal and pathological processes. In this way, high RDW values may warrant some caution in the interpretation of HbA1c results in the laboratory. In our series, a significantly negative correlation in the diabetic population was demonstrated between HbA1c and RDW (p = 0.006; r =–0.182). The latter parameter was increased in the control group compared with the diabetic group, and increased in diabetics with HbA1c < 6.5%, which is consistent with the results of Chinmay et al.[16] This may be explained by the adverse effects of hyperglycemia on erythrocyte survival, or by other abnormalities associated with T2DM (oxidative stress, inflammation, or other components of metabolic syndrome). Thus, as lifespan of erythrocytes is decreased there will be a decrease in HbA1c concentration as the average time during which erythrocytes are exposed to glucose is reduced. Therefore, RDW may represent an indirect measure of hyperglycemia and/or dysmetabolism in this population.
Hyperglycemia has a direct relationship with the development of an inflammatory state. It is responsible for an increased secretion of proinflammatory cytokines such as interleukin-6 and tumor necrosis factor-α. In this case, an anti-erythropoietic effect occurs favoring the apoptosis of immature erythrocytes, which causes a further decrease in the number of circulating erythrocytes, and consequently, a reduction in hemoglobin concentration. In our series, the mean hemoglobin concentration in diabetics was greater than in the control group without being significant (p = 0.568). Hemoglobin in diabetics with good glycemic control was higher than in the group of diabetics with poor glycemic control (p 0.672). Similar results were reported by Afsar and colleagues[17] suggesting that good diabetic control is essential to prevent the development of anemia in diabetic individuals with poor glycemic control.
The MCV is a blood parameter reporting the size of red blood cells, and allows classification of anemia into: microcytic, macrocytic, and normocytic. It has been recently considered as a risk marker for morbidity and mortality for renal and cardiovascular diseases in various study populations, and as a suitable marker for the diagnosis of diabetic nephropathy in patients with T2DM.[18] Our study has objectified significantly decreased values in the diabetic population compared with the nondiabetic population, thus agreeing with the results of Adane et al.[19] This can be explained by the significant effect of oxidative stress related to diabetes on erythrocyte enzymes which can induce a decrease in MCV.[20]
Several platelet parameters are considered to be key indicators of any change in platelet morphology, and therefore help in the early identification of the prothrombotic event, such as PDW, platelet count, platelet volume-to-number ratio, and MPV.[7] The latter parameter of the blood count provides information on the size of platelets. Larger platelets are more physiologically and enzymatically active: they contain more granules, produce greater quantities of vasoactive and thrombotic factors, have a greater capacity to aggregate in response to a stimulus, and express a greater number of adhesion molecules.[21] In our series, all platelet indices were increased in diabetic patients compared with nondiabetic patients, this elevation was not statistically significant except for volume/platelet count (p = 0.023). This is consistent with the results of Nada (p = 0.238) and Akinsegun et al (p = 0.593).[8,22] Our study also showed a nonsignificant elevation of MPV in diabetics with HbA1c levels ≤ 6.5% than in diabetics with HbA1c levels < 6.5% (p = 0.342),[8] which is the case for the series of Nada (p = 0.524).
When correlation tests were performed between MPV and glycemic parameters in our study series, it was observed that there is a significant and positive correlation between MPV and HbA1c in diabetic population (p = 0.006), this joining results of Harsha and Tripati[23] (p < 0.001), Lippi et al[24] (p < 0.001), Razak et al[25] (p = 0.001), Inoue et al[26] (p < 0.005), and Agrawal et al[27] (p = 0. 013).23–27 It can be deduced that good glycemic control decreases the hyperactivity of platelet function and thus may prevent or delay possible diabetic vascular complications. However, our data need to be confirmed by even larger studies.
The limitations of our present study were the qualitative assessment of platelets, as well as their secondary increase, which is seen during menstruation, for example.
The present study has certain limitations. Apart from lack of some individual’s characteristics such as duration of diabetes and the therapeutic aspect of diabetic patients, this is a hospital-based study with small sample size. Therefore, the result of the present study could not be generalized to the population. Furthermore, the cross-sectional nature of this study means that no conclusive results can be drawn as to the actual character and temporality of the correlations observed between the parameters studied.
CONCLUSIONS
Diabetes mellitus is a chronic metabolic disease that requires reproducible and inexpensive means to ensure good glycemic monitoring. In this context, our study showed that RDW correlates negatively and significantly with HbA1c, and may serve as an indirect index of glycemia and dysmetabolism. Inversely, it was observed that MPV is higher in diabetic patients than healthy subjects and is particularly higher in uncontrolled glycemia, with a significant and positive correlation between MPV and HbA1c in diabetic population, which means that improved glycemic control decreases MPV, and consequently recovered platelet functions and activity, and may prevent the possible role of platelets in cardiovascular events in T2DM. However, further studies are also needed to define specific RDW and MPV values predictive of complication risk in the diabetic population.
Note
An earlier presentation was not applicable.
Statement of Institutional Review Board Approval
The members of the research ethics committee reviewed the protocol on May 18, 2023 and according to the Law 28–13 regarding theprotection of persons participating in research: The study is approved (attached letter of approval).
Authors’ Contributions
I.M.: Provided substantial contribution to the conception and design of the study, contributed to the acquisition, analysis and interpretation of data for the work, drafted the manuscript, and gave final approval of the version to be published. L.H.: Specialist in rheumatology with a Master’s degree in SPSS software who helped in the statistical analysis. S.H.: Assisted in determining the exclusion criteria and in the careful selection of eligible patients for the case series study. S.S.: Assisted in the smooth running of preanalytical and analytical phases of the samples intended for the realization of blood counts. AS.A.: Supervised this case series study from conception to interpretation of data and critically revised the work for important intellectual content.
Conflict of Interest
None declared.
References
- Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas. In: Diabetes Res Clin Pract Vol 157. (9th edition). 2019. p. :2000-2006.
- [CrossRef] [PubMed] [Google Scholar]
- International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes | diabetes care. Clin Biochem Rev. 2009;32:1327-1334.
- [CrossRef] [PubMed] [Google Scholar]
- Diabetes mellitus: a review of some of the prognostic markers of response to treatment and management. JInsulResist. 2019;3:222-225.
- [CrossRef] [Google Scholar]
- Endothelial dysfunction and platelet hyperactivity in type 2 diabetes mellitus: molecular insights and therapeutic strategies. Cardiovasc Diabetol. 2018;17:121.
- [CrossRef] [PubMed] [Google Scholar]
- Association of hema-tological indicies with diabetes, impaired glucose regulation and microvascular complications of diabetes. Int J Clin Exp Med. 2015;8:11420-11427.
- [Google Scholar]
- Association between novel inflammatory markers derived from hemogram indices and metabolic parameters in type 2 diabetic men. Aging Male. 2020;23:923-927.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of mean platelet volume in patients with diabetes mellitus, impaired fasting glucose and non-diabetic subjects. Singapore Med J. 2008;49:114-116.
- [Google Scholar]
- Red cell distribution width in type 2 diabetic patients. Diabetes Metab Syndr Obes. 2015;8:525-533.
- [CrossRef] [PubMed] [Google Scholar]
- Some haematological parameters in diabetic patients in Port Harcourt Nigeria. Asian J Multidiscip Stud. 2015;3:21-25.
- [Google Scholar]
- Correlation of hemoglobin A1c with red cell width distribution and other parameters of red blood cells in type II diabetes mellitus. Cureus. 2019;11:e5533.
- [CrossRef] [PubMed] [Google Scholar]
- Red blood cell distribution width and mortality risk in a community-based prospective cohort. Arch Intern Med. 2009;169:588-594.
- [CrossRef] [PubMed] [Google Scholar]
- Red cell distribution width as a novel prognostic marker in heart failure: data from the CHARM Program and the Duke Databank. J Am Coll Cardiol. 2007;50:40-47.
- [CrossRef] [PubMed] [Google Scholar]
- Red blood cell distribution width as a predictor of atrial fibrillation. J Clin Lab Anal. 2018;32:e22378.
- [CrossRef] [PubMed] [Google Scholar]
- Red cell distribution width and risk for first hospitalization due to heart failure: a population-based cohort study. Eur J Heart Fail. 2011;13:1355-1361.
- [CrossRef] [PubMed] [Google Scholar]
- The glycemic status determines the direction of the relationship between red cell distribution width and HbA1c. J Diabetes Complications. 2021;35:108012.
- [CrossRef] [PubMed] [Google Scholar]
- Association of increased levels of glycated hemoglobin with variations in red blood cell parameters in diabetes mellitus. Int J Adv Res (Indore). 2018;4:31-37.
- [Google Scholar]
- Role and significance of hematological parameters in diabetes mellitus. Ann Pathol Lab Med. 2019;6:200-202.
- [CrossRef] [Google Scholar]
- Mean corpuscular volume (MCV): a suitable marker for the diagnosis of diabetic nephropathy in type 2 diabetes mellitus patients. TEXILA Int J Clin Res. 2019;6:32-44.
- [CrossRef] [Google Scholar]
- Red blood cell parameters and their correlation with renal function tests among diabetes mellitus patients: a comparative cross-sectional study. Diabetes Metab Syndr Obes. 2020;13:3937-3946.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of oxidative stress on human red cells glutathione peroxidase, glutathione reductase level, and prevalence of anemia among diabetics. N Am J Med Sci. 2011;3:344-347.
- [CrossRef] [PubMed] [Google Scholar]
- Mean platelet volume increases in type 2 diabetes mellitus independent of HbA1c level. Acta Med Mediter. 2014;30:210-211.
- [Google Scholar]
- Mean platelet volume and platelet counts in type 2 diabetes: mellitus on treatment and non-diabetic mellitus controls in Lagos, Nigeria. Pan Afr Med J. 2014;18:42.
- [CrossRef] [PubMed] [Google Scholar]
- A study on correlation of mean platelet volume with HbA1c in type 2 diabetes mellitus. J Assoc Physicians India. 2023;71:1.
- [Google Scholar]
- The mean platelet volume is significantly associated with higher glycated hemoglobin in a large population of unselected out-patients. Prim Care Diabetes. 2015;9:226-230.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship between mean platelet volume and albuminuria in patients with type 2 diabetes mellitus. Diabetes Metab Syndr. 2019;13:2633-2639.
- [CrossRef] [PubMed] [Google Scholar]
- Association between mean platelet volume in the pathogenesis of type 2 diabetes mellitus and diabetic macrovascular complications in Japanese patients. J Diabetes Investig. 2020;11:938-945.
- [CrossRef] [PubMed] [Google Scholar]
- Mean platelet volume (MPV) the neglected marker of cardiovascular risk and glycosylated hemoglobin in diabetic patient. Diabetes Metab Syndr. 2017;11:109-112.
- [CrossRef] [PubMed] [Google Scholar]





