Translate this page into:
Trends of voluntary reporting of needlestick injuries and hepatitis B vaccination status among health-care workers of a tertiary health care center in Puducherry
Address for correspondence: Dr. Udhayasankar Ranganathan, Department of Microbiology, Sri Manakula Vinayagar Medical College and Hospital, Puducherry - 605 107, India. E-mail: drudhaysnkr@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
BACKGROUND:
Health-care workers (HCWs) can sustain needlestick injuries (NSIs) during patient care activities and are at a greater risk of exposure to blood-borne infectious agents such as HBV, HCV, and HIV, among which only HBV has an effective vaccine. Unfortunately, both the voluntary reporting rates of NSIs and HBV vaccination coverage among HCWs have been generally low. This study aims to analyze the trends of voluntary reporting of NSIs and the HBV vaccination status among the HCWs of our tertiary health care center.
MATERIALS AND METHODS:
A retrospective study was conducted between January 2016 and July 2018 at a tertiary health care center in Puducherry. A standard pro forma was filled by all HCWs reporting NSIs. HIV, hepatitis B virus surface antigen, and hepatitis C virus were tested using rapid card tests, and anti-hepatitis B surface titers were tested using enzyme-linked immunosorbent assay according to the manufacturer's instructions.
RESULTS:
A total of 83 incidents of NSIs were reported. Nursing staffs reported the maximum number of incidents followed by students. About 42 incidents of NSI were reported in the year 2018 compared to 26 and 15 incidents reported in 2017 and 2016, respectively. Only 37 HCWs had taken the complete course of HBV vaccine.
CONCLUSION:
This study shows an increase in the voluntary reporting of NSIs by the HCWs, but the HBV vaccination status among them was found to be low.
Keywords
Health-care workers
hepatitis B vaccination
needlestick injury
Introduction
The National Institute for Occupational Safety and Health, Centers for disease control and prevention(CDC), defines needlestick injuries (NSIs) as “those injuries caused by needles such as hypodermic needles, blood collection needles, intravenous (IV) stylets, and needles used to connect parts of IV delivery systems.”[1] A person in a developing country receives about 3.7 health-care injections per year.[2] About 2 in 35 million health-care workers (HCWs) sustain NSIs every year, putting them at risk of exposure to blood-borne infectious agents, of which HBV, HCV, and HIV constitute a significant proportion, approximately 37%, 39%, and 4.4%, respectively.[3] The risk of transmission of HBV (6%–30%) through NSIs is much higher relative to HCV (1.8%) and HIV (0.3%). Furthermore, among the three important pathogens transmitted through NSIs, only HBV has an effective vaccine. Unfortunately, the voluntary reporting rates of NSIs globally has been low, more so in developing countries where NSIs are more common than the developed world.[4567] The HBV vaccination coverage among HCWs has also been generally low, putting them at greater risk for HBV infections.[8910]
This study intends to analyze the trends of voluntary reporting of NSIs among HCWs and also the HBV vaccination status among those HCWs reporting NSIs in our tertiary health-care center over 30 consecutive months.
Materials and Methods
This is a retrospective study conducted between January 2016 and July 2018 at a tertiary health-care center in Puducherry. Ethical clearance certificate was obtained from the Institutional Ethical Committee (Study no. EC/05/2019 dated January 28, 2019). A standard per forma was filled by all HCWs reporting NSIs and a record of the same was maintained.
Testing for HIV, hepatitis B virus surface antigen (HBsAg), and HCV was offered to the HCWs and also to the sources if known. HIV testing, HBsAg testing, and HCV testing were done using AIDSCAN HIV-1 and 2 Trispot Test Kit manufactured by Bhat Bio-tech India private limited, Alere Trueline Rapid Test Kit for HBsAg manufactured by Alere Medical Private Limited, India, and HCV Tri-Dot manufactured by Diagnostic Enterprises, India, respectively. All the tests were performed and interpreted according to the manufacturer's instructions. The testing for HIV 1 and 2 was done according to the National AIDS Control Organization Guidelines. Anti-HBS titers were tested for those HCWs who have received at least one dose of the HBV vaccine. The test was done using HbsAb enzyme-linked immunosorbent assay kit manufactured by Dia, Pro Diagnostic Bioprobes, Italy, according to the manufacturer instructions. The HCWs were followed up at 6 weeks, 3 months, and 6 months for HIV and at 3 months and 6 months for HBV and HCV, respectively, after counseling and appropriate interventions. The data were entered into an Excel sheet and analyzed.
The hospital infection control committee (HICC) of the institute was also conducting active awareness programs for the prevention of hospital-acquired infections including sessions on NSIs during the study period. The program was conducted every month and comprised two sessions. The number of participants was restricted to a maximum of 25 only, and those participants missing any sessions were advised to attend the same in the subsequent months.
Results
A total of 83 incidents of NSIs were reported between January 2016 and July 2018 by different personnel involved in health care. Among them, 43 incidents were reported by male HCWs and 40 were reported by female HCWs. Nursing staffs reported the maximum number of incidents (37) followed by students (12) and janitors (11) [Figure 1]. About 42 incidents of NSI were reported in the year 2018 compared to 26 and 15 incidents reported in 2017 and 2016, respectively [Figure 2]. Among the sources, 11 were positive for HBsAg, 2 were positive for HIV, 1 was positive for HCV, 57 were negative for all the three, and the source was unknown in 12 events. Among the 83 HCWs, only 37 had taken the complete course of HBV vaccine, whereas 15 had incomplete vaccination and 31 have not taken even a single dose of the vaccine. Among the 15 who had incomplete vaccination, 9 have taken only 2 doses, whereas 6 have taken only one dose of the vaccine.[Table 1] Totally, 52 HCWs have taken at least one dose of HBV vaccine, and among them, only 35 were found to have protective antibody titers (>10 mIU/ml), and the remaining 17 had titers <10 mIU/ml. Fortunately, the HCWs (including the two HCWs exposed to HIV seropositive sources) did not turn seropositive for HIV 1 and 2 in the follow-up tests done after 6 weeks, 3 months, and 6 months after exposure.
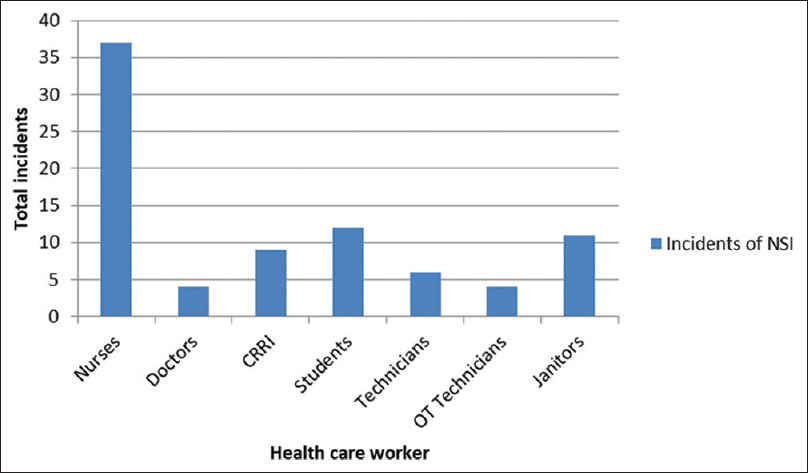
- Total incidents of needlestick injury among various healthcare workers over 30 months
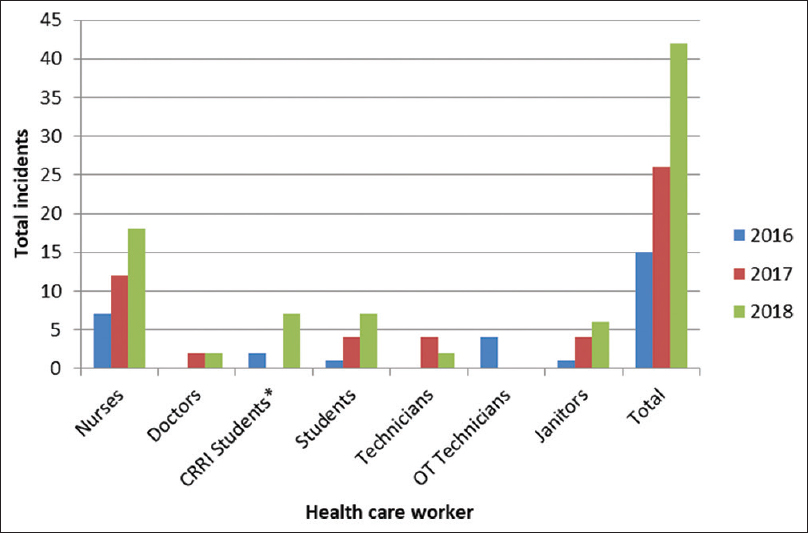
- Trends of voluntary reporting of needlestick injuries over 30 months
| HBV vaccination status | Percentage population |
|---|---|
| Completely vaccinated | 37 (44.6) |
| Incomplete (2 doses) | 15 (18.1) |
| Not vaccinated | 31 (37.3) |
HBV=Hepatitis B virus
Discussion
The health and safety of the workers involved in health care has long been easily overlooked until it got slowly reckoned, and various guidelines related to occupational safety were formulated by different organizations.[11] In spite of the implementation of these guidelines, there is still underreporting of NSIs by HCWs globally. Our study finds overall increasing trends of reporting of NSIs among HCWs of the institute over a period of 30 months.
There was no significant difference in incidents related to the gender of the HCWs. Among the various categories of HCWs, nursing staff reported the maximum number of incidents, whereas reporting by doctors was the least. This may be attributed to the fact that nurses are more prone to NSIs as shown by many studies.[121314]
A gradual increase in the rates of reporting of NSIs is observed in this study. This change in the attitude of the HCWs may be attributed to the frequent conduct of awareness programs by the HICC of the institute. The institute also provides hepatitis B vaccination to all its HCWs at zero cost despite adding to its economic burden. The WHO, apart from recommending organizations to make policies and periodic education of staffs on safe injection practices such as avoiding recapping of syringes and applying universal precautions to prevent NSIs, also suggests providing alternates to injection and modifying the mechanics of sharp operation.[15] Implementing all these may also significantly add to the economic burden of the organization. Nevertheless, a systematic review about the economic evaluation of NSIs has shown that, though NSIs contribute to the economic burden of the organization, the measures aimed at preventing the same could prove to be beneficial in the long run.[16]
We found that nearly 38% of individuals were found to be unvaccinated and 18% were found to be incompletely vaccinated against HBV. This state of low vaccination coverage against HBV among HCWs is also seen in different parts of the world, as shown by many studies.[1718] Studies conducted at various health centers in India also show that a high proportion of its HCWs were not vaccinated against HBV.[1920]
Between 18% of those incompletely vaccinated in this study, none had anti-hepatitis B antibody titers more than 10 mIU/ml, putting them at higher risk for HBV infections. These findings suggest that health-care providers should be appraised about the importance of complete vaccination against HBV and the health hazards of hepatitis B virus infections.
Conclusion
This study shows an increase in the voluntary reporting of NSIs by HCWs. The HBV vaccination status among the HCWs was found to be low.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Available from: https://www.cdc.gov/niosh/docs/2000108/default.html
- Best infection control practices for intradermal, subcutaneous, and intramuscular needle injections. Bull World Health Organ. 2003;81:491-500.
- [Google Scholar]
- Sharps injuries: Assessing the burden of disease from sharps injuries to healthcare workers at national and local levels 2005. Available from: https://www.who.int/quantifying_ehimpacts/publications/ebd11/en/
- [Google Scholar]
- Needle stick injuries among health care workers in a tertiary care hospital of India. Indian J Med Res. 2010;131:405-10.
- [Google Scholar]
- Prevalence and reporting of needle stick injuries: A survey of surgery team members in Kermanshah university of medical sciences in 2012. Glob J Health Sci. 2015;8:245-51.
- [Google Scholar]
- The incidence and reporting rates of needle-stick injury amongst UK surgeons. Ann R Coll Surg Engl. 2009;91:12-7.
- [Google Scholar]
- Epidemiology of needlestick and sharp injuries among health care workers based on records from 252 hospitals for the period 2010-2014, Poland. BMC Public Health. 2019;19:634.
- [Google Scholar]
- A cross-sectional study on hepatitis B Vaccination status and post-exposure prophylaxis practices among health care workers in teaching hospitals of Mangalore. Ann Glob Health. 2015;81:664-8.
- [Google Scholar]
- Hepatitis B vaccination coverage among healthcare workers at national hospital in Tanzania: How much, who and why? BMC Infect Dis. 2017;17:786.
- [Google Scholar]
- Attitude and vaccination status of healthcare workers against hepatitis B infection in a teaching hospital, Ethiopia. Scientifica (Cairo). 2018;2018:6705305.
- [Google Scholar]
- Healthcare workers: Protecting those who protect our health. Infect Control Hosp Epidemiol. 1997;18:397-9.
- [Google Scholar]
- Needle stick injuries among health care workers in tertiary care hospital in tertiary care hospital of rural India. Int J Med Sci Public Health. 2014;3:49.
- [Google Scholar]
- Needle stick injuries and their related safety measures among nurses in a university hospital, Shiraz, Iran. Saf Health Work. 2016;7:72-7.
- [Google Scholar]
- Prevalence of needle-stick injuries among health-care workers in a tertiary care centre in North India. J Patient Saf Infect Control. 2018;6:45.
- [Google Scholar]
- Preventing needle stick injuries among healthcare workers: A WHO-ICN collaboration. Int J Occup Environ Health. 2004;10:451-6.
- [Google Scholar]
- How much do needlestick injuries cost? A systematic review of the economic evaluations of needle stick and sharps injuries among healthcare personnel. Infect Control Hosp Epidemiol. 2016;37:635-46.
- [Google Scholar]
- Hepatitis B vaccination coverage in healthcare workers in Gauteng Province, South Africa. Vaccine. 2011;29:4293-7.
- [Google Scholar]
- Hepatitis B vaccination coverage among health care workers in China. PLoS One. 2019;14:e0216598.
- [Google Scholar]
- Prevalence of hepatitis B virus infection in healthcare workers of a tertiary care centre in India and their vaccination status. J Vaccines Vaccin. 2011;2:118.
- [Google Scholar]





