Translate this page into:
Florid Erythrophagocytosis on the Peripheral Smear
Address for correspondence: Dr. Vani Chandrashekar, E-mail: drvani001@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Erythrophagocytosis is a relatively rare observation on blood smears. It has been reported in auto immune hemolytic anemias and sporadically in few other conditions. Here, we report a case of florid erythrophagocytosis with severe anemia following a viral infection in an 18-year-old girl. Her complete blood count (CBC) revealed hemoglobin of 3.6 gm/dl and a hematocrit of 10%. The peripheral smear showed erythrophagocytosis by neutrophils and rosetting of erythrocytes around neutrophils. The direct Coombs test and direct Donath- Landsteiner tests were positive.
Keywords
Autoimmune hemolytic anemia
Donath-Landsteiner test
erythrophagocytosis
paroxysmal cold hemoglobinuria
INTRODUCTION
Cold antibody-mediated autoimmune hemolytic anemias encompass both cold agglutinin syndrome and paroxysmal cold hemoglobinuria (PCH).[1] Cold agglutinin syndrome affects predominantly middle aged or elderly whereas PCH typically presents in the young, especially children.[1] PCH is mediated by cold reactive biphasic IgG autoantibody. It is directed against the P blood group antigen on red cell membranes. It binds to red blood cells and fixes complement at low temperatures (0-4°C) in the extremities. At 37°C in the central circulation these RBCs undergo intravascular lysis due to activation of the complement cascade by the classical pathway. Clinically the patient presents with acute onset of fever, pallor, jaundice, and hemoglobinuria. There is severe anemia and erythrophagocytosis on the peripheral smear. Neutrophil erythrophagocytosis has been reported as a prominent feature of PCH.[2–4] Adherence of RBCs to and rosetting around neutrophils have also been reported in PCH.[5]
Erythrophagocytosis has been reported sporadically following spider bite,[6] quinine administration,[7] and in hemolytic diseases of the newborn.[8] Erythrophagocytosis by cells other than neutrophils has been reported in acute myeloid leukemia,[9] in blast crisis of chronic myeloid leukemia[10] and occasionally in warm autoimmune hemolytic anemia.
Paroxysmal cold hemoglobinuria has been reported from different parts of the world and there have been sporadic reports from India in syphilitic patients and in children.[1112]
There is scarcity of reports of PCH from India and we hope to increase the awareness of clinicians and pathologists to the importance of this treatable cause of severe anemia.
CASE REPORT
An 18-year-old female patient presented to the medical outpatient department with complaints of high grade fever, vomiting post food intake, and passing high coloured urine for the past three to four days. She gave history of multiple vesicles on her body along with fever, which occurred around ten days prior to the onset of her presenting complaints. These vesicles first appeared on the back and then spread to her face and limbs. She was not on any medication.
On examination, she was remarkably pale, febrile, and icteric. She was conscious and oriented. There was tachypnoea and tachycardia with no organomegaly. A complete blood count revealed a haemoglobin of 3.6 gm/dl, a hematocrit of 10%, a total leucocyte count of 10100/cumm, and a platelet count of 2,94000/cumm. The red cell mean corpuscular volume (MCV) was 93.1fl, mean corpuscular haemoglobin (MCH) 42.7 pg, and mean corpuscular haemoglobin concentration (MCHC) 45.8 gm/dl. The RBC count was 0.77 million/cumm. The peripheral smear was remarkable for erythrophagocytosis by more than 50% of the neutrophils with rosetting of RBCs around neutrophils [Figures 1, 2]. Polychromasia and RBC agglutination with occasional nucleated RBCS were seen. There was no toxic granulation seen in the neutrophils. Reticulocytosis was present with a reticulocyte percentage of 9.5. The sample was incubated at 37°C and MCV, MCH, MCHC, and RBC count of the incubated sample was 89.1 fl, 31.6 pg, 35.5 gm/dl, and 1.05 million/cumm, respectively. Her total bilirubin level was 4.5 mg/dl of which, direct bilirubin was 1.1 mg/dl and indirect bilirubin 3.4 mg/dl. Serum lactate dehydrogenase was 3887 IU/l. Her urine was high coloured with a specific gravity of 1.25 and presence of protein (1+, 50 mg/dl). Urine microscopy showed yellowish brown granular casts (2-3/hpf) and 3-4 epithelial cells/hpf. No red cells were seen in the sediment. The direct Coombs test was strongly positive for c3d and negative for IgG. However, cold agglutinin titre was not elevated. The direct Donath-Landsteiner test was positive, conclusive of PCH. She was transfused with packed red cells and treated symptomatically.
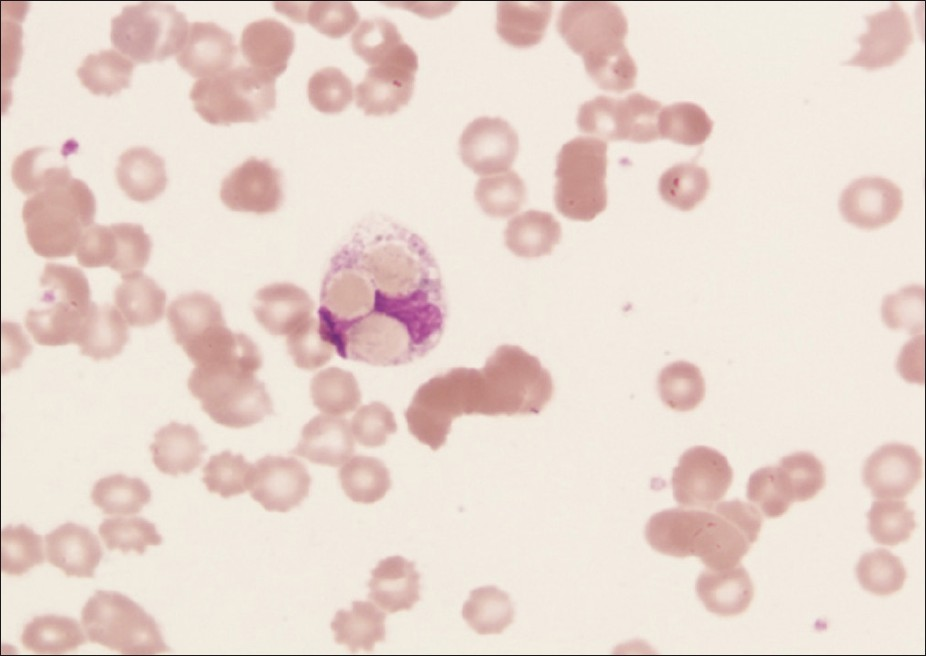
- Neutrophil with erythrophagocytosis
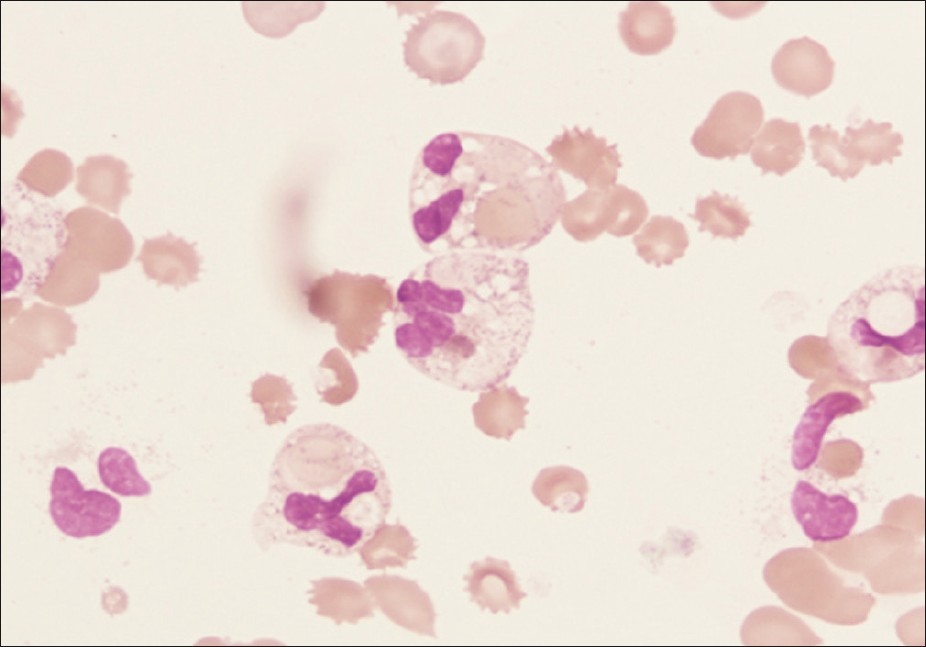
- Erythrophagocytosis in many neutrophils
On the second day, her haemoglobin was 3.4 gm/dl with reticulocytosis, a leucoerythroblastic blood picture and marked erythrophagocytosis by neutrophils. During her stay in hospital she was transfused with packed red cells and treated symptomatically.
She was discharged on the tenth day after admission when her haemoglobin had risen to 9 gm/dl. The peripheral smear demonstrated erythrophagocytosis in occasional neutrophils. On follow-up, a month later, her haemoglobin was 11 gm/dl, with no erythrophagocytosis and a serum lactate dehydrogenase level of 350 IU/l.
DISCUSSION
PCH was considered an unusual disease till recently. Now it is considered as a most common cause of acute autoimmune haemolytic anaemia in children.[13] PCH classically presents in the young with acute onset of fever, malaise, abdominal pain, jaundice, marked pallor, and high colored urine. Previously, secondary PCH was reported in association with latent syphilis. With effective therapy for syphilis, this association is now, rare. PCH is now linked to chicken pox,[1415] measles,[16] mumps,[17] upper respiratory tract infection,[18] and Hemophilus influenza.[19]
Our patient, a young female presented with a severe anaemia and high colored urine following a viral exanthem. There were scabs on her trunk which were consistent with chicken pox infection. Serological tests for antibody titres were however not available. Her haemoglobin was 3.6 gm/dl with reticulocytosis, RBC agglutination, and marked erythrophagocytosis by neutrophils. Following symptomatic treatment and blood transfusion her haemoglobin improved to 9 gm/dl and the peripheral smear showed erythrophagocytosis in a rare neutrophil only.
There was RBC agglutination on the peripheral smear, which could indicate a cold agglutinin syndrome. However, acute presentation of severe anaemia in a young patient following infection is unlikely in cold agglutinin syndrome. Further, the marked erythrophagocytosis by neutrophils support a diagnosis of PCH. This is confirmed by the positive direct Donath-Landsteiner test. The treatment options and prognosis for both these conditions vary and hence diagnosis is mainstay of treatment.
This case highlights the importance of erythrophagocytosis in diagnosis of PCH and the necessity for clinicians to be aware of this condition when a patient with a viral exanthem develops sudden severe anaemia.
ACKNOWLEDGEMENTS
The authors would like to thank Ms Malini C and Mr. Marudhupandian for their efforts.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Erythrophagocytosis in paroxysmal cold hemoglobinuria. Am J Hematol. 2003;74:196-7.
- [Google Scholar]
- Erythrophagocytosis by segmented neutrophils in paroxysmal cold hemoglobinuria. Am J Clin Pathol. 1984;81:787-9.
- [Google Scholar]
- Erythrophagocytosis on the peripheral blood smear and paroxysmal cold hemoglobinuria. Transfusion. 2001;41:1073-4.
- [Google Scholar]
- Spider bite hemolytic anemia: Positive Coombs test, erythrophagocytosis and leukoerythroblastic smear. Am J Clin Pathol. 1984;81:683-7.
- [Google Scholar]
- Erythrophagocytosis and thrombocytopathy occurring during the course of a Henoch- Schonlein syndrome due to quinine. Am J Med. 1954;17:423-31.
- [Google Scholar]
- Erythrophagocytosis in hemolytic disease of the newborn. Am J Hematol. 2008;83:679.
- [Google Scholar]
- Near-tetraploid minimally differentiated acute myeloid leukemia with extensive erythrophagocytosis by leukemic blasts. Ann Hematol. 2000;79:36-9.
- [Google Scholar]
- Phagocytosis of hematopoietic cells by blast cells in blast crisis of chronic myelocytic leukemia. West J Med. 1977;126:139-41.
- [Google Scholar]
- Paroxysmal cold haemoglobinuria.The most frequent acute autoimmune haemolytic anaemia in children? Acta Paediatr Scand. 1984;73:258-62.
- [Google Scholar]
- Paroxysmal cold haemoglobinuria in an adult with chicken pox. Br J Haematol. 2000;109:328-9.
- [Google Scholar]
- A case of paroxysmal cold haemoglobinuria following chickenpox. Ceylon Med J. 2010;55:96.
- [Google Scholar]
- Recurrent paroxysmal cold haemoglobinuria in a 3-year-old child: A case report. Transfus Med. 2003;13:319-21.
- [Google Scholar]
- Transfusion medicine illustrated: Donath-Landsteiner antibody-associated hemolytic anaemia after Haemophilus influenzae infection in a child. Transfusion. 2004;44:1127-8.
- [Google Scholar]





