Translate this page into:
Comparison of calculated versus directly-measured low-density lipoprotein-cholesterol: An evaluation of ten formulas for an HIV-positive population in Sub-Saharan Africa
Address for correspondence: Dr. Ifeyinwa Osegbe, Department of Chemical Pathology, University of Nigeria Teaching Hospital, Ituku/Ozalla, Enugu State, Nigeria. E-mail: ifeyinwa.osegbe@unn.edu.ng
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
BACKGROUND:
Low-density lipoprotein cholesterol (LDLC) is a modifiable risk factor for atherosclerotic cardiovascular disease, therefore needs to be assessed and monitored. Direct homogeneous assays and various formulas exist to determine LDLC. We aimed to compare the directly measured LDL (dLDLC) with ten formulas for estimating LDLC.
MATERIALS AND METHODS:
This was a 2-year retrospective study of fasting lipid profile results obtained from HIV-positive patients attending an outpatient clinic at the University of Nigeria Teaching Hospital, Enugu, Nigeria, using homogeneous direct assays. Estimated LDLC was determined using ten formulas. Pearson's correlation, Bland–Altman plots, and linear regression were performed. Statistical significance was P < 0.05.
RESULTS:
Three thousand four hundred and eighty-two lipid results with mean ± standard deviation (SD) dLDLC of 2.1 ± 1.1 mmol/L were included in this study. There was a strong, positive correlation between Friedewald's LDLC and dLDLC n = 3412, r = 0.84, P < 0.001, but linear regression demonstrated a proportional bias P = 0.005. Ahmadi's equation showed the worst correlation n = 3482, r = 0.35, P < 0.001, but when applied to samples with triglyceride (TG) <1.13 mmol/L (100 mg/dl), the correlation showed a strong, positive relationship n = 1395, r = 0.80, P < 0.001, and no proportional bias P = 0.86. Teerankanchana's equation was the only formula that showed no difference between its LDLC and dLDLC (n = 3482, P = 0.056). It also demonstrated strong, positive correlation (n = 3482, r = 0.84, P < 0.001) and had a mean difference ± SD of −0.68 ± 0.63.
CONCLUSION:
Teerankanchana's formula showed good correlation and minimal bias with dLDLC at all TG levels. Moreover, linear regression showed no difference in the two. It seems to be the most suitable formula for estimating LDLC in our HIV-positive population.
Keywords
Cardiovascular disease
Friedewald's equation
low-density lipoprotein cholesterol
Introduction
Low-density lipoprotein cholesterol (LDLC) plays a prominent role in atherosclerotic cardiovascular disease (ASCVD), which is a leading cause of death worldwide.[1] When oxidized, small dense LDL particles are formed, which are engulfed by macrophages to form foam cells, the origin of an atheromatous plaque.[2] At an LDLC blood concentration of 100 mg/dl, some havoc has already commenced, therefore lowering it has been targeted by the National Cholesterol Education Program (NCEP) Adult Treatment Panel as a significant approach to mitigating the prevalence of coronary heart disease.[3]
HIV-positive patients are living longer with the advent of antiretroviral therapy but are now at increased risk for ASCVD due to the high prevalence of dyslipidemia in them as a result of viral and antiretroviral factors.[45] Dyslipidemia characterized by elevated total cholesterol (TC), LDL-cholesterol (LDLC), triglyceride (TG), and reduced HDL-cholesterol (HDLc) is a common feature described in the highly active antiretroviral therapy (HAART)-associated morphologic and metabolic abnormality syndrome or HIV-associated lipodystrophy syndrome,[6] but it is also seen in treatment-naïve patients.[4]
The Friedewald formula (LDLC = TC−HDLc−TG/5) to determine the concentration of LDLC in mg/dl[7] is widely used in various laboratories because it has been well validated across several populations and is cost-effective although it is limited when TG >400 mg/dl.[7] A study by Evans et al. reported as much as 69% of their HIV-infected individuals on antiretroviral therapy had TG ≥400 mg/dl.[8] Due to this limitation, HIV-positive patients may be unfit for the application of this formula because high TG blood level is a common finding in HIV patients receiving protease inhibitor (PI) antiretroviral medication.[910] Therefore, other formulas need to be identified and evaluated.
Directly measured LDLC (dLDLC) is ideal in diagnosing dyslipidemia. Beta-quantification following ultra-centrifugation is the reference method to directly determine LDLC,[11] but it is very expensive and not readily available in diagnostic laboratories. Homogeneous assays which do not require pretreatment have been developed by manufacturers for routine determination of dLDLC,[12] albeit costly as well.
Based on the high cost of dLDLC assays, formulas still have to be considered in resource-limited African laboratories, where HIV still has a prevalence 4.9% equating to 23.5 million people.[13] There is a need to identify an equation that will provide an appropriate surrogate of dLDLC which is not limited by lipid levels (e.g., TG >400 mg/dl). Application of the simple, readily available and cost-effective formula should lead to the early intervention of dyslipidemia in this population preventing ASCVD.
Several formulas for estimating LDLC have been developed and assessed in various populations.[14] Few have been conducted on HIV-positive populations, but none in this environment. Therefore, we aimed to evaluate ten formulas identified in literature versus dLDLC determined from a homogeneous assay.
Materials and Methods
Study design
This was a retrospective study of the serum lipid profile results of HIV-positive patients for 2 years.
Study population
This study was conducted at the HIV outpatient clinic of the University of Nigeria Teaching Hospital (UNTH), Ituku-Ozalla, Enugu state; a 400-bed tertiary health institution in the Southeast Nigeria. Subjects included were male and female adults aged 18–60 years, with confirmed HIV seropositivity by double ELISA and Western blot, who had received HAART for a minimum of 6 months if eligible. Children and patients with secondary causes of dyslipidemia, for example, obesity, hypothyroidism, nephrotic syndrome, Type II diabetes mellitus, pregnant women, and nursing mothers were excluded from the study.
This study was reviewed and approved by the Health Research and Ethics Committee of the UNTH (NHREC/05/01/2008B-FWA00002458-1RB00002323). Consent was obtained from the medical records department of the HIV outpatient clinic to access the patients’ laboratory records and case files. Confidentiality of the patient information was maintained.
Data collection
The medical records of the subjects were reviewed to obtain their lipid profile results, demographics, clinical, and HAART medication history. As per the standard operating procedure of the laboratory, serum samples for lipid profile had been obtained from the subjects after an overnight 10–12 h fast. The samples were allowed to clot and retract before centrifuging at 4000 rpm for 10 min to obtain the serum. Sera were analyzed daily using enzymatic methods for TC,[15] HDLc,[16] and TG,[17] while LDLC was determined by a direct, homogeneous assay,[18] on a Roche Hitachi 902 Autoanalyzer (Roche Diagnostics, Germany).
Data were entered onto a Spreadsheet (Microsoft office Excel 2010, Washington USA). The lipid results were converted from mmol/L to mg/dl and LDLC was calculated using each of the formulas stated by Friedewald,[7] de Cordova and de Cordova,[19] Ahmadi et al.,[20] Hattori et al.,[21] Saiedullah et al.,[22] Anandaraja et al.,[23] Vujovic et al.,[24] Puavilai and Laoragpongse,[25] Chen et al.,[26] and Teerakanchana et al.[27] noting each formulas limitation.
Statistical analysis
Statistical analyses were performed using the IBM SPSS statistics version 20 (Chicago, Illinois, USA). Kolmogorov–Smirnov test was used to check normality of the data and descriptive statistics were presented as mean and standard deviation (SD). Student's t-test was used to compare the means of dLDLC and each calculated LDLC. Pearson's correlation was used to determine the relationship, while Bland–Altman plots were used to demonstrate bias graphically. Linear regression was performed to determine the level of agreement between dLDLC and each of the calculated LDLC, or if there is a proportional bias. The level of statistical significance was established at P < 0.05.
Results
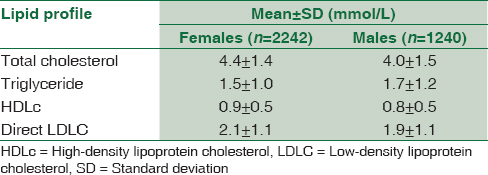
Three thousand four hundred and eighty-two lipid results from 2242 (64.4%) females and 1240 (35.6%) males [Table 1] with mean ± SD age of 37.6 ± 9.4 years and 44.1 ± 10.2 years, respectively, were included in this study. Their median (interquartile range) CD4 count was 244 (106–435) and 171 (60–335) for females and males, respectively. Two thousand three hundred and three (66%) subjects had received nucleoside reverse transcriptase inhibitors (NRTI) + nonnucleoside reverse transcriptase inhibitors (NNRTI) medication, 17 (0.5%) received NRTI + PI medication, 1075 (31%) were ineligible for HAART because their CD4 count was optimal (<350 cells/µl), while there was no documentation of HAART use in 87 (2.5%) of them.
Our study showed strong, positive correlations between dLDLC and all calculated LDLC, but Anandaraja's formula showed the best correlation n = 3482, r = 0.86, P < 0.001 [Table 2]. Ahmadi's equation had the worst correlation r = 0.35, P < 0.001, but when applied to samples with TG < 1.13 mmol/L, the correlation showed a strong, positive relationship n = 1395, r = 0.80, P < 0.001 [Table 2].
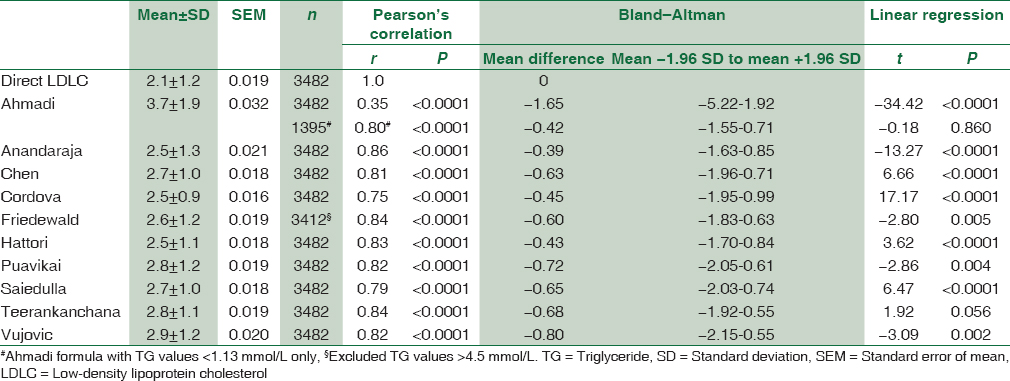
Although all the calculated LDLC showed a negative bias on Bland–Altman graphs, Anandaraja's formula had the least bias with a mean difference ± SD of −0.39 ± 0.63. While on linear regression, Teerankanchana's equation was the only formula that showed no difference between its LDLC and dLDLC (n = 3482, P = 0.056). It also had demonstrated strong, positive correlation (n = 3482, r = 0.84, P < 0.001) and had a mean difference ± SD of −0.68 ± 0.63 [Table 2].
Only 2% of our subjects had TG >4.5 mmol/L, the others n = 3412 (98%) showed a strong, positive correlation between Friedewald's LDLC and dLDLC, r = 0.84, P < 0.001. The mean difference ± SD was −0.60 ± 0.63, but the linear regression demonstrated a proportional bias P = 0.005.
Ahmadi had no proportional bias for samples with TG <1.13 mmol/L, n = 1395, P = 0.86 [Table 2].
Discussion
Homogeneous assays for the direct measurement of LDLC have been critically assessed against the calculation method and have succeeded in attaining the NCEP requirements for LDLC testing which include: Imprecision (CV <4%), inaccuracy (bias <4%), and total allowable error not exceeding ±12%.[28] Likewise, the homogeneous enzymatic colorimetric assay used in this study had also been evaluated against the reference beta-quantification method by and shown to meet the currently established analytical and clinical performance goals for direct LDLC measurement.[18] However, they have questionable reliability and specificity, especially in the presence of atypical lipoproteins.[28]
Friedewald's equation is the most widely used formula in estimating LDLC, but it cannot be applied when TG >4.5 mmol/L (i.e., >400 mg/dl) because it is inaccurate in estimating LDLC at that level.[7] This equation uses TG to estimate the concentration of very LDLC (VLDLC) in serum. Therefore, when TG is in excess, it overestimates VLDLC and underestimates LDLC. To overcome this limitation, patients are required to undergo a 10–12 h fast prior to testing to enable clearance of TG from the blood. Conversely, in patients with Type III hyperlipoproteinemia, where cholesterol predominates because of the division of TG by the factor 5, it yields a falsely low VLDLC and a falsely high LDLC.[29]
Based on the above limitations, Friedewald's equation is not recommended to determine LDLC in Type II diabetics,[30] hepatic failure,[31] and end-stage renal disease patients,[32] as well as HIV-positive patients on HAART, especially PI[10] because they are characterized by hypertriglyceridemia. Our study showed that only seventy (2%) of our subjects who had been on HAART for at least 6 months presented with TG >4.5 mmol/L. This may be because the majority of our subjects (66%) had received NRTI and NNRTI medication, versus 0.5% who received PI. In Nigeria, PI is the second-line antiretroviral therapy which is administered only when NRTI and NNRTI regimens fail.[33]
In our study, dLDLC and Friedewald LDLC were not in agreement, but a study conducted on HIV-infected individuals by Evans et al.[8] showed that both direct enzymatic LDLC (Genzyme®) and Friedewald LDLC did not agree with the reference ultracentrifugation method with increasing TG levels because the former overestimates LDLC while the latter underestimates it; likely due to lack of precision when TG <400 mg/dl, but the direct assay was still more beneficial.[8]
Ahmadi et al. demonstrated another limitation of Friedewald's equation stating that strong correlations do not exist at TG <1.13 mmol/L (i.e., <100 mg/dl), thereby recommending their formula.[20] Our study corroborates that when using all TG values, correlation of dLDLC to Ahmadi LDLC was poor, n = 3482, r = 0.35; but when we selected samples with TG <1.13 mmol/L, correlation was strong-positive, n = 1395, r = 0.80. Moreover, there was no statistically significant difference between dLDLC and Ahmadi LDLC at these levels, n = 1395, P = 0.860.
Cordova's equation claims to be useful in nonfasting states[19] because TG is not required in the formula. Since TG is the greatest concern in HIV specimens, it is expected that this formula should be the best suited for this population. However, our study differed from this hypothesis by demonstrating the weakest correlation with dLDLC (n = 3482, r = 0.75) compared to the other formulas, and it has a proportional bias with dLDLC.
Saiedulla's formula claims to be best for TG >1000 mg/dl (i.e., 11.3 mmol/L),[22] which would be a desirable equation since our homogeneous assay has a negative bias of 10% when TG >1000 mg/dl,[18] but our study did not observe any subject with this concentration of TG in their specimen to test this. This may suggest that HIV-positive patients in our environment do not develop such high levels of hypertriglyceridemia, unlike in other settings where TG values ranging up to 3000 mg/dl have been reported.[8]
Anandaraja et al. evaluated their equation against Friedewald and dLDLC using ultracentrifugation and beta-quantification, but still concluded that Friedewald was in better agreement with dLDLC.[23] Our study used homogeneous assay to determine dLDLC, and observed that Anandaraja's formula had a better correlation than Friedewald (n = 3482, r = 0.86 vs. n = 3412, r = 0.84) and showed the least bias on Bland–Altman graph (mean difference = −0.39) compared to other equations.
Despite these, Teeranchana's LDLC showed good correlation with minimal bias, and the linear regression showed no difference between the two methods. Only when TG <1.13 mmol/L is Ahmadi's equation recommended.
This study was limited by the retrospective study design as it was impossible to control patients’ preparation, specimen collection, and analysis. As well as assess the analytical performance of the dLDLC assay. We had to rely on the compliance to standard operating procedures utilized by the laboratory and quality control records of their analytical system.
Conclusion
Equations for estimating LDLC may need to be applied in HIV-positive populations in sub-Saharan Africa because of its simplicity and lower cost. Our study showed Teerankanchana's formula was not different from direct LDLC at all levels of TG, but Ahmadi was a better option when TG <1.13 mmol/L. Although limited by the retrospective nature of this study, these two formulas are potentials for calculating LDLC in our HIV-positive population, but further studies using more robust direct homogeneous assays for comparison are needed to confirm this.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 2011. World Health Organization. Causes of Death 2008: Data Sources and Methods. Available from: http://www.who.int/healthinfo/global_burden_disease/cod_2008_sources_methods.pdf
- Blood vessels. In: Kumar V, Abbas AK, Fausto N, eds. Robbins and Cotran Pathologic Basis of Disease (7th ed). Pennsylvania: Elsevier, Saunders; 2005. p. :511-54.
- [Google Scholar]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486-97.
- [Google Scholar]
- HIV infection and high density lipoprotein metabolism. Atherosclerosis. 2008;199:79-86.
- [Google Scholar]
- Association of serum lipid levels with HIV serostatus, specific antiretroviral agents, and treatment regimens. J Acquir Immune Defic Syndr. 2007;45:34-42.
- [Google Scholar]
- Human immunodeficiency virus (HIV) disease: AIDS and related disorders-diseases of the endocrine and metabolic disorders. In: Harrison's Principles of Internal Medicine (15th ed). New York: McGraw-Hill; 2001.
- [Google Scholar]
- Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499-502.
- [Google Scholar]
- A Study Team. Comparison of direct and indirect measurement of LDL-C in HIV-infected individuals: ACTG 5087. HIV clin trials. 2007;8:45-52.
- [Google Scholar]
- Dyslipidaemia in HIV-infected patients: Association with adherence to potent antiretroviral therapy. Int J STD AIDS. 2001;12:463-8.
- [Google Scholar]
- Hyperlipidemia associated with protease inhibitor therapy. Ann Pharmacother. 1999;33:859-63.
- [Google Scholar]
- Optimization of beta-quantification methods for high-throughput applications. Clin Chem. 2001;47:712-21.
- [Google Scholar]
- Seven direct methods for measuring HDL and LDL cholesterol compared with ultracentrifugation reference measurement procedures. Clin Chem. 2010;56:977-86.
- [Google Scholar]
- 2012. Joint United Nations Programme on HIV/AIDS (UNAIDS). 2012 UNAIDS Report on Global AIDS Epidemic. Available from: http://www.unaids.org/en/resources/documents/2012/20121120_UNAIDS_Global_Report_2012
- Calculated low density lipoprotein cholesterol: Friedewald's formula versus other modified formulas. Int J Life Sci Med Res. 2014;4:25-31.
- [Google Scholar]
- Direct measurement of high-density lipoprotein cholesterol in serum with polyethylene glycol-modified enzymes and sulfated alpha-cyclodextrin. Clin Chem. 1995;41:717-23.
- [Google Scholar]
- Quantitative determination of serum triglycerides by the use of enzymes. Clin Chem. 1973;19:476-82.
- [Google Scholar]
- Analytical and clinical performance of a detergent-based homogeneous LDL-cholesterol assay: A multicenter evaluation. Clin Chem. 2000;46:506-14.
- [Google Scholar]
- A new accurate, simple formula for LDL-cholesterol estimation based on directly measured blood lipids from a large cohort. Ann Clin Biochem. 2013;50(Pt 1):13-9.
- [Google Scholar]
- The impact of low serum triglyceride on LDL-cholesterol estimation. Arch Iran Med. 2008;11:318-21.
- [Google Scholar]
- Development of approximate formula for LDL-chol, LDL-apo B and LDL-chol/LDL-apo B as indices of hyperapobetalipoproteinemia and small dense LDL. Atherosclerosis. 1998;138:289-99.
- [Google Scholar]
- A simple modification of Friedewald's formula to calculated low density lipoprotein cholesterol up to serum triglyceride concentration of 1000mg/dl. Bangladesh J Med Biochem. 2009;2:62-5.
- [Google Scholar]
- Low-density lipoprotein cholesterol estimation by a new formula in Indian population. Int J Cardiol. 2005;102:117-20.
- [Google Scholar]
- Evaluation of different formulas for LDL-C calculation. Lipids Health Dis. 2010;9:27.
- [Google Scholar]
- Is calculated LDL-C by using the new modified Friedewald equation better than the standard Friedewald equation? J Med Assoc Thai. 2004;87:589-93.
- [Google Scholar]
- A modified formula for calculating low-density lipoprotein cholesterol values. Lipids Health Dis. 2010;9:52.
- [Google Scholar]
- Comparative study of LDL-cholesterol levels in Thai patients by the direct method and using the Friedewald formula. Southeast Asian J Trop Med Public Health. 2007;38:519-27.
- [Google Scholar]
- Methods for measurement of LDL-cholesterol: A critical assessment of direct measurement by homogeneous assays versus calculation. Clin Chem. 2002;48:236-54.
- [Google Scholar]
- Calculated values for low-density lipoprotein cholesterol in the assessment of lipid abnormalities and coronary disease risk. Clin Chem. 1990;36:36-42.
- [Google Scholar]
- Accuracy of calculated serum low-density lipoprotein cholesterol for the assessment of coronary heart disease risk in NIDDM patients. Diabetes Care. 1998;21:1397-402.
- [Google Scholar]
- Is the determination of LDL cholesterol according to Friedewald accurate in CAPD and HD patients? Clin Nephrol. 1996;46:319-25.
- [Google Scholar]
- Limitations of the Friedewald formula for estimating low-density lipoprotein cholesterol in alcoholics with liver disease. Clin Chem. 1994;40:404-6.
- [Google Scholar]
- Federal Ministry of Health. Guidelines for the Use of Antiretroviral (ARV) Drugs in Nigeria. Abuja: Federal Ministry of Health; 2007. p. :38-41.





